Hashimoto’s Thyroiditis Treatment: Addressing the Therapeutic Void with New Alternatives
Aug 04, 2025
Hashimoto’s thyroiditis is an autoimmune disorder in which the immune system mistakenly attacks the thyroid gland, leading to persistent inflammation, gland enlargement, and the development of autoantibodies targeting thyroid proteins. Formerly known as “struma lymphomatosa,” it is now recognized as the leading cause of hypothyroidism and is linked to an increased risk of cardiovascular conditions and certain cancers. The onset of the disease is shaped by a combination of genetic susceptibility, environmental influences, and epigenetic changes.
From an epidemiological perspective, Hashimoto’s thyroiditis is one of the most common thyroid disorders, with a higher incidence in women of all ages. However, its true prevalence is frequently underestimated in clinical evaluations, as autopsy studies reveal a wider presence of thyroid autoimmunity than previously recognized. This gap highlights the need for greater awareness and vigilance, particularly in at-risk populations.
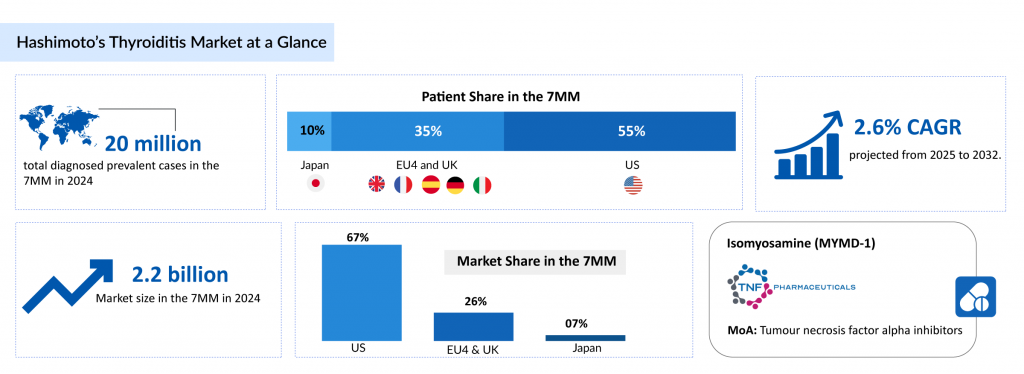
According to DelveInsight, approximately 20 million diagnosed prevalent cases of Hashimoto’s thyroiditis were reported across the 7MM in 2024, with the United States accounting for about 55% of these. Based on cytological findings, Hashimoto’s thyroiditis is classified into different types, including the euthyroid form (asymptomatic), which made up around 5 million US cases in 2024, followed by clinical hypothyroidism (symptomatic) and subclinical hypothyroidism (asymptomatic).
Downloads
Click Here To Get the Article in PDF
Recent Articles
Current Hashimoto’s thyroiditis treatment options are limited, as no approved therapies specifically target its autoimmune origins. This therapeutic gap underscores the pressing need for novel interventions that can prevent thyroid damage, mitigate disease progression, and enhance long-term patient outcomes.
Challenges in the Hashimoto’s Thyroiditis Therapeutic Landscape
The current approach to managing Hashimoto’s thyroiditis is largely symptomatic, combining both drug-based and lifestyle interventions to handle its multifaceted nature. As there is no known cure, treatment is centered around easing symptoms, improving patients’ quality of life, and slowing disease progression. Therapies are tailored to address the specific manifestations of the condition.
Pharmacological management depends on the severity of the disease, with different strategies for subclinical versus overt hypothyroidism. Levothyroxine (LT4) remains the gold standard for treating overt hypothyroidism, especially in symptomatic individuals, and is also considered for some subclinical cases. LT4 helps restore normal thyroid hormone levels, which are essential for metabolic regulation, energy balance, and cognitive health, thereby relieving both physical and mental symptoms.
Despite these treatments, options for Hashimoto’s thyroiditis remain limited, as there are no therapies that can cure or alter the course of the disease. Current methods offer only symptomatic relief and do not halt progression. The lack of early and accurate diagnostic tools further delays intervention, compounding the disease’s impact.
Introducing a novel therapy that targets the root causes of Hashimoto’s thyroiditis could revolutionize disease management. Such an advancement would offer new hope to patients and caregivers, potentially leading to rapid adoption, enhancement of clinical guidelines, and expansion of the treatment landscape, shifting the paradigm from symptom control to long-term, sustainable care.
Hashimoto’s Thyroiditis Pipeline: Limited Options, One Hope
The treatment pipeline for Hashimoto’s thyroiditis remains limited, with Isomyosamine (MYMD-1) from TNF Pharmaceuticals standing out as the primary candidate. This reflects a significant opportunity to develop more targeted therapies.
Isomyosamine (MYMD-1) is an oral selective inhibitor of Tumor Necrosis Factor-alpha (TNF-α), a key driver of chronic inflammation in autoimmune disorders. Unlike conventional TNF-α inhibitors that broadly dampen immune function, MYMD-1 is designed to selectively inhibit TNF-α only when it becomes excessively active, such as in autoimmune thyroiditis or cytokine storms, while preserving its essential immune role during normal infections.
The drug also exhibits anti-fibrotic and anti-proliferative properties, broadening its potential application to diseases involving tissue scarring and abnormal cell growth. Its oral formulation offers a significant benefit over currently available TNF-α inhibitors, which require injection or intravenous delivery.
In September 2021, Phase I clinical trial data for MYMD-1 in Hashimoto’s thyroiditis were submitted to the U.S. FDA as part of the annual IND update. Based on the findings, the FDA offered guidance for proceeding to Phase II trials.
The anticipated launch of this emerging therapy are poised to transform the Hashimoto’s thyroiditis treatment landscape in the coming years. As more of these cutting-edge therapies continue to mature and gain regulatory approval, they are expected to reshape the Hashimoto’s thyroiditis treatment landscape, offering new standards of care and unlocking opportunities for medical innovation and economic growth.
Future Outlook of Hashimoto’s Thyroiditis Treatment Space
The future of Hashimoto’s thyroiditis treatment is poised to move beyond traditional hormone replacement therapy, driven by a growing understanding of the disease’s autoimmune basis. While levothyroxine remains the standard of care for hypothyroidism caused by Hashimoto’s thyroiditis, it does not address the underlying immune dysregulation. According to DelveInsight’s analysis, the Hashimoto’s thyroiditis market in the 7MM was valued at USD 2.2 billion in 2024. Over the forecast period from 2025 to 2034, this market is projected to grow at a CAGR of 2.6%.
Emerging therapies aim to modify or halt the autoimmune process altogether, with research focusing on immune modulators, T-cell therapies, and agents targeting pro-inflammatory cytokines such as TNF-alpha.
Another promising direction is the integration of precision medicine approaches, including genomic and microbiome profiling, to identify patients who may benefit from tailored immunomodulatory interventions. Studies suggest that gut dysbiosis and genetic polymorphisms may contribute to disease onset and severity.
By stratifying patients based on their molecular or microbiome profiles, future therapies could be more effectively personalized, improving both efficacy and tolerability. Additionally, bioinformatics tools and AI-driven diagnostics are being explored to detect early autoimmune activity, allowing for earlier intervention before irreversible thyroid damage occurs.
Looking ahead, combination therapies and preventive strategies could reshape the Hashimoto’s thyroiditis treatment paradigm. These may include combining low-dose immunosuppressants with thyroid hormone replacement or utilizing tolerogenic vaccines that retrain the immune system to tolerate thyroid antigens.
Advances in biologics, RNA-based therapies, and cellular therapies also hold potential to induce long-term remission. Ultimately, the future of Hashimoto’s thyroiditis management will likely center around disease-modifying therapies that go beyond symptom control, aiming instead to preserve thyroid function and improve long-term patient outcomes.

Downloads
Article in PDF



