Artificial Intelligence in Remote Patient Monitoring: Enabling Continuous, Predictive, and Personalized Care
Oct 15, 2025
Table of Contents
The convergence of Artificial Intelligence (AI) and Remote Patient Monitoring (RPM) marks a pivotal shift toward predictive, continuous, and patient-centric healthcare. As chronic diseases rise globally, healthcare systems are under pressure to deliver timely, personalized interventions without overburdening hospital infrastructure. Here, AI-driven RPM emerges as a transformative solution, integrating real-time data analytics, sensor fusion, and predictive modeling to enhance care delivery, optimize clinical decisions, and improve outcomes across diverse populations.
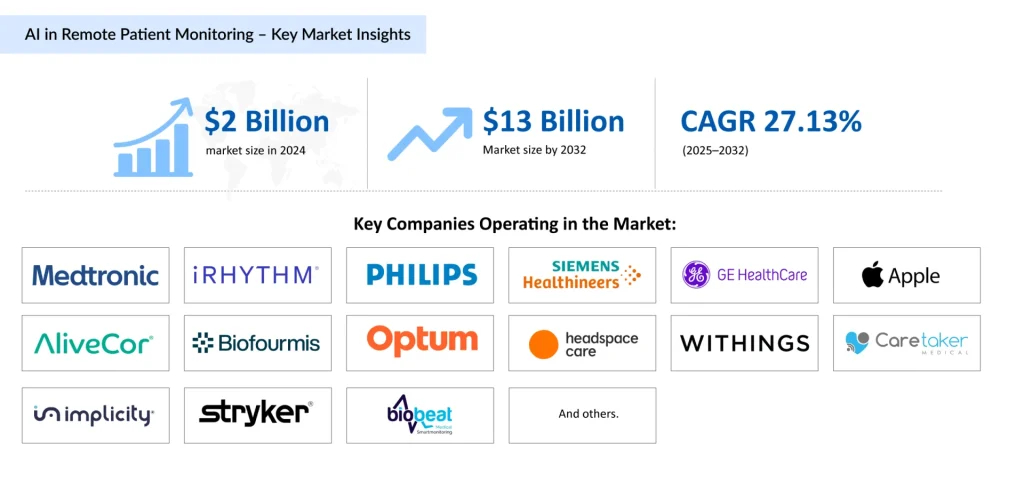
The AI in Remote Patient Monitoring market was valued at ~USD 2 billion in 2024, projected to grow at a CAGR of 27.13% from 2025 to 2032, reaching ~USD 13 billion by 2032. This explosive growth reflects a paradigm shift from reactive to proactive healthcare, driven by increasing chronic disease prevalence, expanding wearable adoption, and the rapid evolution of AI-powered analytics. North America leads this revolution, supported by strong digital infrastructure, widespread use of connected medical devices, and government-backed telehealth initiatives.
Downloads
Click Here To Get the Article in PDF
Recent Articles
- iVEAcare’s $27.5 Million Series A Funding; AI Medical Service Joint Research Agreement with Mahid...
- Medtronic Diabetes Secures FDA Clearance for MiniMed Go™ Smart MDI Platform; Neurolief Achieves F...
- Navigating U.S. Tariffs in 2025: Impacts and Strategies for Pharma and Healthcare
- Wearing Technology to stay fit
- Liso-cel (lisocabtagene maraleucel) Shines in Second-Line, Yielding Long-Lasting Complete Respons...
This article explores how AI in remote patient monitoring is redefining healthcare delivery, from chronic disease management to post-operative recovery, while analyzing the latest innovations, academic and industrial breakthroughs, and the ethical frameworks shaping this next frontier in digital health.
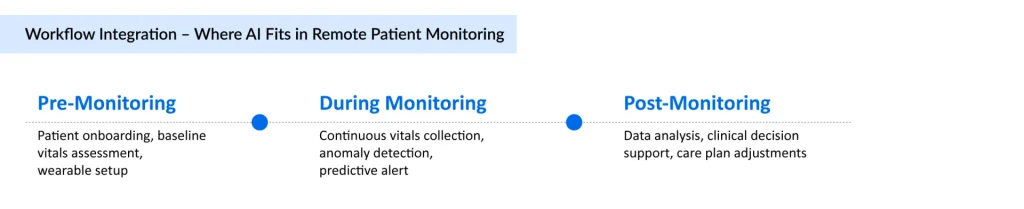
The Rise of AI-Powered Remote Patient Monitoring
Over the past decade, remote patient monitoring has evolved from basic telemetric tracking to sophisticated, AI-enabled ecosystems capable of continuous learning and adaptive insights. Traditional RPM systems, though valuable, were limited by static thresholds and manual interpretation of data. AI now bridges these gaps by recognizing subtle physiological patterns, predicting health deterioration before symptoms surface, and empowering clinicians to intervene early.
The surge in AI in remote patient monitoring is driven by multiple converging forces:
- The global rise in chronic diseases such as cardiovascular disorders, diabetes, respiratory illnesses, and cancer which demand long-term, real-time surveillance.
- Advances in wearable sensors and IoT devices, generating continuous data streams on heart rate, oxygen saturation, blood pressure, temperature, and movement.
- 5G and edge computing, enabling ultra-low-latency data transmission and on-device intelligence.
- Healthcare system digitalization, which integrates electronic health records (EHRs), imaging, and lab data for holistic patient views.
AI algorithms convert these vast, multidimensional data into actionable insights. Machine learning models detect anomalies in vitals, forecast readmission risks, and optimize care plans, while natural language processing (NLP) integrates unstructured clinical notes into predictive dashboards.
Leading health technology firms, including Medtronic, iRhythm Inc., Koninklijke Philips N.V., Siemens Healthineers, GE HealthCare, Apple, alivecor Inc., Biofourmis, Optum, Headspace Health, Withings, NeuroRPM, Caretaker Medical, Implicity, Stryker, Biobeat, are at the forefront of integrating AI with connected monitoring platforms to detect arrhythmias, respiratory distress, and neurological anomalies in real time. Their solutions are complemented by startups and academic collaborations introducing new models for adaptive, privacy-conscious monitoring.
Current Challenges in Traditional Remote Monitoring Systems
Despite widespread adoption, conventional RPM systems face intrinsic limitations that hinder clinical scalability and predictive accuracy.
Data Overload and Interpretation Bottlenecks:
Continuous data streams from wearables and sensors generate massive datasets. Manual or threshold-based monitoring often leads to alert fatigue, missed anomalies, and delayed intervention.
Fragmented Integration:
Many RPM solutions operate in silos, disconnected from EHR systems, laboratory data, or imaging results. This fragmentation prevents clinicians from obtaining a complete health profile, reducing contextual accuracy.
Limited Predictive Capability:
Traditional systems rely on static thresholds, detecting deviations only after they occur. Without predictive analytics, early detection of conditions like heart failure or sepsis remains limited.
Accessibility and Inequity:
High device costs, lack of digital literacy, and inadequate connectivity in low-resource settings restrict the reach of RPM technologies, especially among aging and rural populations.
Privacy and Compliance Concerns:
Continuous data collection raises questions about security, patient consent, and compliance with HIPAA, GDPR, and other data protection laws.
Addressing these challenges requires an infusion of AI at every level, from intelligent data filtering and adaptive learning to real-time anomaly prediction and automated clinical decision support.
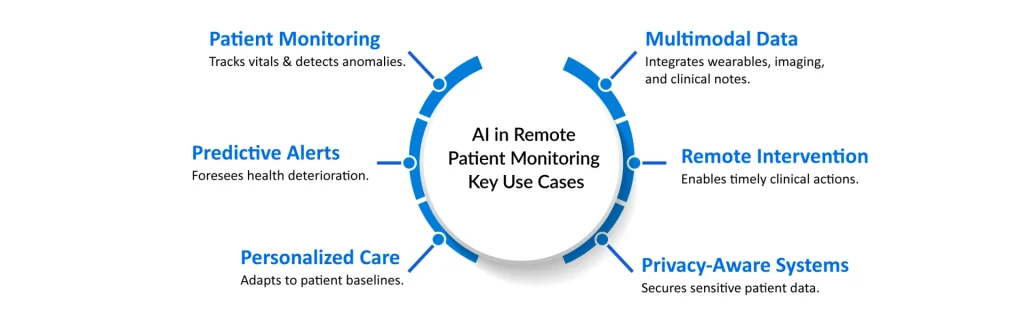
How AI is Transforming the Remote Monitoring Landscape
The integration of Artificial Intelligence in Remote Patient Monitoring is re-architecting healthcare delivery. AI systems now provide clinicians with predictive insights, automate alert triage, and enable early interventions that can prevent hospitalizations and improve patient outcomes.
Predictive Analytics and Early Intervention
AI models analyze longitudinal health data to identify subtle deviations before critical deterioration occurs. For example, deep learning algorithms trained on ECG and SpO₂ data can detect early signs of heart failure, enabling preventive therapy adjustments.
A January 2025 study proposed a deep learning model that detects hypertension anomalies from wearable data, improving early cardiovascular risk warnings (Frontiers, 2025). Similarly, an AI-powered stethoscope by Eko Health and Imperial College London identifies heart valve disease, arrhythmias, and heart failure in 15 seconds, validated across 12,000+ patients (The Guardian, August 2025).
Personalized and Adaptive Monitoring
AI-driven systems continuously adapt to patient baselines. Unlike static thresholds, they learn individual physiological patterns, reducing false positives and increasing specificity. The RECOVER System (February 2025) introduced an LLM-based RPM platform for post-GI cancer surgery patients, combining chatbot-based symptom tracking with an intelligent dashboard. This system improved patient adherence and enabled clinicians to personalize post-operative care.
Multimodal Data Integration
Modern AI-RPM frameworks combine sensor, imaging, behavioral, and contextual data for holistic health assessment. For instance, IoT-driven RPM systems for cardiovascular care integrate ECG, blood pressure, and SpO₂ in real-time, and have been tested successfully on clinical populations in Pakistan.
Privacy-Aware AI Systems
Privacy remains central to RPM evolution. A 2025 arXiv study proposed a privacy-aware eHealth system using radar sensing and semantic communication, minimizing data transmission while maintaining continuous monitoring accuracy. Such innovations address ethical concerns by ensuring that AI insights do not compromise patient confidentiality.
Real-Time Risk Stratification and Clinical Decision Support
AI models provide clinicians with continuous risk scores, flagging anomalies like arrhythmias, respiratory decline, or glucose spikes in real-time dashboards. Cleveland Clinic and Piramidal unveiled an AI EEG model that monitors ICU brain activity to detect seizures and neurological decline, trained on 1 million+ hours of EEG data.
These advances demonstrate AI’s power not just to monitor patients but also to actively support physicians in prioritizing high-risk cases and allocating resources efficiently.
Key Applications of AI Across Remote Monitoring Domains
AI’s versatility allows it to be deployed across diverse clinical settings and diseases, supporting a continuum of care beyond hospital walls.
Cardiovascular Monitoring
AI-enhanced ECG and photoplethysmography (PPG) algorithms detect arrhythmias, atrial fibrillation, and heart failure decompensation early. Platforms like iRhythm’s Zio and Eko AI leverage continuous monitoring to predict cardiac events before they occur, reducing hospital readmissions by up to 25% in clinical trials.
Diabetes and Metabolic Disorders
AI models analyze continuous glucose monitoring (CGM) data, dietary logs, and activity metrics to personalize insulin dosing and predict glycemic fluctuations. These systems enable automated alerts for hypoglycemia or hyperglycemia, enhancing self-management and adherence.
Oncology and Post-Surgical Care
AI-RPM systems such as RECOVER track post-operative symptoms, vitals, and patient-reported outcomes after cancer surgeries. Predictive algorithms detect infection risks or wound complications early, allowing remote interventions and reducing hospital stays.
Respiratory and Sleep Disorders
AI analyzes breathing patterns, oxygen saturation, and acoustic data to detect COPD exacerbations, sleep apnea, and asthma attacks. Coupled with smart inhalers or connected oxygen devices, such systems improve disease control and reduce emergency visits.
Neurology and Mental Health
Continuous EEG and wearable-based AI systems detect seizure risks or cognitive decline in real time. Emerging models also analyze voice, speech patterns, and facial cues to detect mood disorders and depression, paving the way for neuro-RPM integration.
Notable Case Studies and Breakthroughs
The shift from conceptual to applied AI in RPM is evident in both academia and industry.
- Royal Philips + smartQare Partnership (April 2024): Integrated viQtor with Philips’ patient monitoring platforms to enable next-generation continuous monitoring in hospitals and remotely, initially in Europe.
- Dozee (India, December 2024): Deployed contactless AI-RPM at AJ Hospital, Mangalore, using sensors to track HR, RR, SpO₂, and temperature with automated alerts, improving ICU capacity and early deterioration detection.
- AI Early-Warning RPM (Kolkata, October 2024): A scalable, privacy-respecting model for continuous monitoring in urban hospitals, showcasing India’s growing presence in digital health innovation.
- iRhythm Technologies Zio® ECG (September 2024): Received Japanese regulatory approval for the first AI-powered arrhythmia monitoring service.
- 5G + AI Hybrid Systems (January 2025): Achieved 14.4 ms latency and 96.5% accuracy in vital prediction, enabling near-real-time care.
- Real-Time Anomaly Detection Models (February 2025): AI frameworks using secure communications to detect anomalies in continuous monitoring, targeted for clinical deployment.
- Eko Health’s AI Stethoscope (August 2025): Accurately detects cardiac abnormalities in seconds, proving the viability of AI-enabled diagnostic monitoring.
- Cleveland Clinic + Piramidal (August 2025): Launched an AI EEG system for continuous ICU monitoring, transforming neurocritical care with predictive seizure alerts.
Collectively, these breakthroughs confirm that AI-enabled monitoring is not a futuristic concept but a practical, scalable solution delivering measurable clinical value today.
Regulatory and Ethical Considerations
As AI becomes embedded in clinical workflows, regulators and healthcare providers must ensure compliance, fairness, and transparency.
Data Privacy and Security
RPM data is inherently sensitive. Adhering to HIPAA, GDPR, and ISO/IEC 27001 standards is essential. Modern systems employ federated learning, training AI models across distributed datasets without transferring personal information, to maintain both accuracy and privacy.
Algorithmic Transparency and Bias Mitigation
AI models must be interpretable to clinicians. Black-box algorithms risk eroding trust, especially when influencing life-critical decisions. Regulators now encourage the use of explainable AI (XAI), enabling a transparent rationale behind alerts or predictions.
Informed Consent and Patient Autonomy
Patients should understand how their data is used, stored, and processed. RPM platforms increasingly use interactive digital consent models that clarify AI’s role in monitoring and decision-making.
Regulatory Oversight
Authorities such as the FDA and European Medicines Agency (EMA) are advancing guidance on AI/ML-based Software as a Medical Device (SaMD). AI-RPM solutions must demonstrate analytical validity, clinical performance, and ongoing monitoring post-deployment to maintain certification.
The Transformative Future of AI in Remote Patient Monitoring
The next decade will redefine RPM from passive data collection to predictive, personalized, and preventive care ecosystems powered by continuous AI intelligence.
Predictive and Preventive Health
By combining genomics, real-world evidence, and sensor data, AI will shift care from reactive treatment to proactive prevention. Algorithms will not only detect but also forecast health events, from arrhythmias to respiratory collapse.
Integration with Digital Twins
Digital twin technology, virtual replicas of patients built on multimodal data, will simulate physiological responses, allowing clinicians to test treatment scenarios and personalize interventions without risk.
Voice and Behavioral Analytics
Future AI systems will incorporate speech tone, gait, and micro-expressions as digital biomarkers for neurological and psychiatric conditions, broadening RPM’s diagnostic reach.
Edge AI and On-Device Processing
To address latency and privacy issues, AI computation will increasingly move to the device level, reducing reliance on cloud transmission and enabling instant analytics, particularly in rural or low-bandwidth regions.
Seamless Integration with Smart Homes and Hospitals
RPM will evolve into “ambient health ecosystems,” where smart homes equipped with AI sensors monitor residents’ wellness passively, sharing data with care teams via secure networks.
Policy and Value-Based Care Integration
Payers and governments are beginning to reimburse AI-RPM services, recognizing their potential to reduce hospital admissions and overall healthcare costs. These incentives will drive adoption, particularly for chronic disease management.
The Future is Predictive, Connected, and Compassionate
Artificial Intelligence in Remote Patient Monitoring is more than a technological evolution, it represents a philosophical transformation of healthcare. By turning continuous data into foresight, AI empowers clinicians to intervene before crises, enables patients to take control of their wellness, and ensures that healthcare becomes not just reactive but predictive and equitable.
With global investments accelerating, academic innovation thriving, and ethical frameworks maturing, the next decade will see AI-RPM emerge as a cornerstone of precision health. The fusion of AI, connectivity, and compassion promises a healthcare future that is intelligent, inclusive, and profoundly human.

Downloads
Article in PDF
Recent Articles
- Chimeric Antigen Receptor T cell Therapy Market
- The AI Drug Discovery Revolution: Smarter Science, Faster Therapies, Better Outcomes
- Wireless Brain Sensors: Revolutionizing Neuroscience and Healthcare
- New cancer drug tested in mice may benefit certain leukaemia patients
- Byondis’s HER2-targeting ADC trastuzumab duocarmazine; AbbVie Migraine Drug Atogepant; Grünenthal...