FDA Approved Expanded Indication for Max 3™ Syringeless MR Injector from Bracco
On November 25, 2025, Bracco Diagnostics Inc., the U.S. subsidiary of Bracco Imaging S.p.A., announced that the U.S. Food and Drug Administration (FDA) expanded the indication for its Max 3™ Rapid Exchange and Syringeless Injector for use in MRI procedures. The system, which had already been cleared for single-dose and multi-dose vials, was now also authorized for use with the newly approved VUEWAY® (gadopiclenol) Injection Imaging Bulk Package (IBP) in 30 mL and 50 mL formats.
The Max 3™ injector, recognized as the first and only syringeless MRI injector in the U.S. market, had been engineered to provide precise, efficient, and hygienic contrast delivery. It streamlined MRI contrast administration via an intuitive, guided user interface that enabled technologists to perform studies more quickly and reliably. Its adaptable design supported both traditional single-use vials and multi-dose IBPs, allowing hospitals to optimize workflow, handle high patient volumes, and work toward sustainability goals.
The FDA’s approval of Bracco’s VUEWAY® IBP offered hospitals a new option to enhance workflow efficiency and reduce waste when using an FDA-cleared automated contrast injector such as Max 3™. The multi-dose packaging enabled multiple single doses to be delivered from a single container, ensuring aseptic handling, minimizing material waste, and improving the overall utilization of contrast agents.
VUEWAY® (gadopiclenol), administered intravenously, provided effective MRI contrast enhancement at half the gadolinium dose of other macrocyclic GBCAs for U.S.-approved indications, offering added patient and environmental advantages. By this point, more than three million VUEWAY® injections had been administered across over 902 customer sites, reflecting its expanding role in high-quality MR imaging.
This milestone also highlighted Bracco’s ongoing commitment to innovation and environmental responsibility. The company had implemented sustainable manufacturing practices, including energy-efficient upgrades and reverse osmosis systems. It continued to develop products to reduce gadolinium exposure, reduce plastic waste, and lower the environmental impact of diagnostic imaging.
“This expanded presentation to our VUEWAY® product line and the Bracco MR family of MRI solutions underscores Bracco’s ongoing commitment to advancing performance, efficiency, and sustainability in MRI contrast delivery,” said Gary Ray, Associate Director, MR Marketing, Bracco Americas. “These innovations reflect our mission to empower hospitals with flexible solutions that reduce waste, streamline workflow, and uphold the highest standards of quality and sterility across the imaging suite.”
According to DelveInsight’s “Magnetic Resonance Imaging (MRI) Devices Market Report,” the magnetic resonance imaging devices market was valued at USD 8,207.06 million in 2024, growing at a CAGR of 6.54% from 2025 to 2032 to reach USD 13,553.33 million by 2032. The rising prevalence of various chronic disorders, such as cardiovascular diseases, cancer, and neurological conditions, is fueling the demand for precise diagnostic tools like MRI, which offers superior imaging capabilities for soft tissues and organs. Additionally, the increasing awareness and the emphasis on early diagnosis of chronic disease are encouraging patients and healthcare providers to adopt MRI for timely intervention. Furthermore, technological advancements play a crucial role in boosting the MRI market, with innovations such as high-field and open MRI systems, functional MRI (fMRI), and faster scan times improving the accuracy, comfort, and efficiency of the imaging process. Collectively, these factors are expected to increase global demand for magnetic resonance imaging devices during the forecast period from 2025 to 2032.
RapidAI Extended the Reach of Deep Clinical AI with Five New FDA Clearances
On November 25, 2025, RapidAI, a pioneer in deep clinical AI and a global leader in enterprise imaging, announced that the U.S. Food and Drug Administration (FDA) had cleared five new imaging modules: Rapid DeltaFuse™, Rapid LMVO, Rapid MLS, Rapid OH, and Rapid Aortic, marking a major expansion of the Rapid Enterprise™ Platform. These clearances reinforced RapidAI’s position as the only platform designed to deliver deep clinical intelligence, seamless workflow integration, and secure IT infrastructure across hospitals worldwide.
The company had long focused on developing deep clinical AI capable of detecting more diseases, reducing radiologists’ cognitive workload, supporting acute treatment and transfer decisions, and improving long-term patient management. To achieve this, RapidAI developed algorithms that went beyond simple triage, enabling physicians to characterize, quantify, visualize, and track disease progression over time. The newly cleared modules highlighted this commitment by strengthening clinical decision-making across the entire patient journey rather than just at the initial diagnostic step.
Rapid DeltaFuse was developed to support long-term patient follow-up by automatically aligning and co-registering serial non-contrast head CT scans, helping clinicians visualize subtle changes, such as hemorrhages, masses, or ventricular shifts. Studies have shown that it reduced radiologist comparison time by more than 36%.
Rapid LMVO provided complete brain coverage on CTA, including anterior, posterior, basilar, and distal territories, enhancing RapidAI’s leadership in ischemic stroke imaging. Together with its perfusion and non-contrast modules, it offered the only fully validated CT- and MRI-perfusion-based stroke solution supported by randomized clinical trials.
Rapid MLS detected and quantified a suspected midline shift with high precision, achieving a mean absolute error of just 0.8 mm, helping clinicians identify critical brain injuries earlier.
Rapid OH identified suspected obstructive hydrocephalus by detecting cerebrospinal fluid accumulation in the ventricles and delivered alerts in under one minute, improving triage and transfer workflows. It also qualified for CMS NTAP, reflecting its clinical and economic value.
Rapid Aortic analyzes any CT scan, including the aorta, to help clinicians identify, measure, and monitor aortic pathology. It provided guideline-based measurements, automated 3D reconstructions, longitudinal comparisons, and follow-up notifications, thereby improving surveillance consistency and reducing physician workload.
Overall, these FDA clearances strengthened RapidAI’s comprehensive AI ecosystem, enhanced its clinical utility across neurology and cardiovascular care, and expanded its role in supporting hospital workflows and patient management.
“The FDA clearances of these solutions underscore our commitment to deep clinical AI and reducing cognitive burden for radiologists, as well as supporting superior decision-making and outcomes,” said Karim Karti, CEO of RapidAI. “RapidAI algorithms help set new standards by enabling radiologists to practice at the top of their license, reducing cognitive burden, and improving clinical decision-making for better outcomes in both acute and long-term settings.”
As per DelveInsight’s “Artificial Intelligence (AI) in Medical Imaging Market Report,” the global artificial intelligence in medical imaging market is expected to increase from USD 1,673.03 million in 2024 to USD 13,181.93 million by 2032, growing at a CAGR of 29.48% during the forecast period from 2025 to 2032. The global artificial intelligence in medical imaging market is being driven by the rising prevalence of chronic diseases such as cancer, cardiovascular disorders, and neurological conditions, which increase demand for accurate and efficient diagnostics. Government initiatives and funding are promoting healthcare digitization and AI adoption, while key players are investing in product development and strategic collaborations to enhance imaging solutions. Rapid advancements in deep learning, machine learning, and computer vision are further improving diagnostic accuracy, workflow efficiency, and predictive capabilities, collectively accelerating market growth across regions.
Ceribell Received FDA 510(k) Clearance for use of Clarity® Algorithm for Neonates
On November 24, 2025, CeriBell, Inc., a medical technology company dedicated to advancing the diagnosis and management of severe neurological conditions, announced that the U.S. Food and Drug Administration (FDA) had granted 510(k) clearance for its next-generation Clarity® algorithm. This advanced AI-driven algorithm is designed to detect electrographic seizures in newborns, including pre-term infants, and older patients. With this clearance, the Ceribell System becomes the first and only AI-powered, point-of-care EEG technology capable of identifying electrographic seizures across all age groups, from pre-term neonates to adults.
Early seizure identification remains a major unmet need in neonatal medicine. Although an estimated 9% of NICU patients are diagnosed with seizures, research shows that as many as 90% may go unnoticed without EEG monitoring. Consequently, a large proportion of high-risk infants could benefit from wider EEG screening. However, many NICUs are still unable to provide timely EEG access or continuous monitoring, leading to avoidable transfers, delayed treatment, and poorer outcomes. Evidence indicates that high-risk newborns experiencing more than 13 minutes of seizure activity within an hour face an eight-fold higher likelihood of adverse outcomes, including mortality or long-term developmental disability. Reinforcing the urgency of prompt intervention, updated guidelines from the American Clinical Neurophysiology Society recommend continuous EEG monitoring for neonates at elevated seizure risk due to conditions such as hypoxic-ischemic encephalopathy, congenital heart disease, and prematurity.
The latest 510(k) clearance is supported by EEG data from over 700 patients, making it the largest known validation dataset for a neonatal seizure detection technology. Ceribell has also previously secured 510(k) clearance for a neonatal-specific headcap. Together, the specialized hardware and proprietary algorithms enable real-time detection of non-convulsive seizures in neonatal patients, supporting rapid clinical decision-making and helping reduce the risk of significant brain injury.
“Seizures are the most common neurological emergency in newborns, and protecting these fragile brains is essential to their long-term development and well-being,” said Jane Chao, Ph.D., co-founder and CEO of Ceribell. “This FDA clearance enables us to further expand availability of Ceribell’s rapid, AI-powered neurological monitoring technology and serve more patients in need. Every newborn deserves timely and accessible seizure detection, without the delays and transfers that too often put outcomes at risk.”
“Ceribell’s easy-to-use, AI-powered point-of-care EEG helps address a critical gap in neonatal care by enabling prompt bedside neurological assessment and delivering real-time insights about each patient’s condition,” said Dr. Janene Fuerch, Medical Director of Neonatal ECMO at Stanford Children’s Hospital. “I have seen firsthand that many NICUs do not have 24/7 access to EEG. There is a clear need for faster, more accessible tools to evaluate brain activity at the bedside – especially in those critical first hours of life.”
As per DelveInsight’s “Electroencephalography Devices Market Report,” the global electroencephalography devices (EEG) system market was valued at USD 1,050.48 million in 2023, growing at a CAGR of 9.96% during the forecast period from 2024 to 2030, to reach USD 1,850.84 million by 2030. The increasing figures of neurological disorders such as epilepsy, stroke, coma, sleeping disorders, and others are primarily boosting the demand for EEG devices. Further, the rising adoption of advanced and innovative technologies, the increasing geriatric population, the expanding device launches & approvals, and others are contributing to the overall growth of the EEG devices market during the forecast period from 2024 to 2030.
BD Surgiphor™ Surgical Wound Irrigation System Expanded to Europe to Help Hospitals Improve Patient Safety
On November 24, 2025, BD (Becton, Dickinson and Company), a global leader in medical technology, announced the launch of the BD Surgiphor™ Surgical Wound Irrigation System in Europe, marking the first system of its kind to receive Conformité Européenne (CE) approval. The product became available in select European countries and was introduced as a sterile, ready-to-use surgical irrigation solution designed to loosen and remove debris from wounds during procedures. By flushing out contaminants, including microorganisms, the system helped reduce bacterial load, a major contributor to surgical site infections.
Rian Seger, worldwide president of BD Surgery, stated that the European launch represented a significant advancement in surgical care, noting that surgical site infections remained a major challenge for patient outcomes and healthcare systems. Surgiphor™, he emphasized, supported clinicians with evidence-based irrigation practices to reduce risk, improve recovery, and enhance overall surgical safety.
Surgiphor™ differed from traditional irrigation methods because it was premixed, sterile, and required no preparation, thereby reducing the preoperative workload. It utilized a trusted antiseptic preservative to help lower bacterial burden and featured an easy-to-handle design that enabled surgical teams to apply it quickly and accurately. By streamlining irrigation and cutting preparation time, the system helped hospitals improve efficiency while supporting safer surgical outcomes. The launch further underscored BD’s ongoing commitment to delivering practical, proven solutions that prioritize patient safety.
According to DelveInsight’s “Wound Irrigation Systems Market Report,” the market for wound irrigation systems is being driven by several strong factors that are steadily increasing demand across hospitals, surgical centers, and emergency care settings. Rising global surgical volumes, particularly in orthopedics, trauma, cardiovascular, and general surgery, are significantly increasing demand for effective intraoperative wound-cleansing solutions that minimize contamination and reduce the risk of surgical site infections (SSIs). The growing incidence of traumatic injuries, burns, chronic wounds, and diabetic ulcers is also expanding the use of irrigation systems in acute and chronic wound management. Increasing clinicians’ awareness of the importance of proper wound decontamination, along with stricter infection-control protocols and guidelines, is further accelerating adoption. Technological advancements, such as ready-to-use sterile solutions, pressure-controlled irrigation devices, and systems designed to improve precision and reduce bacterial load, are making these products more efficient and user-friendly, encouraging wider adoption. Additionally, the rising economic burden of SSIs, pressure from healthcare regulators to reduce hospital-acquired infections, and the shift toward evidence-based surgical practices are reinforcing the need for advanced wound irrigation solutions, collectively driving strong market growth.
Neurophet and The Florey Strengthen Research Collaboration on ‘Neurophet AQUA’ to Advance Alzheimer’s Disease Diagnosis
On November 25, 2025, Neurophet, an AI solution company specializing in brain disorder diagnosis and treatment, announced that it had entered into a research collaboration with the Florey Institute of Neuroscience and Mental Health (The Florey) in Australia, using its neurodegeneration imaging analysis software, Neurophet AQUA.
The joint study, titled “Enhanced Dementia Diagnosis (EDD) in Australian Memory Clinics),” was designed to assess the clinical utility of blood-based and other biomarkers for diagnosing and managing Alzheimer’s disease, with Neurophet AQUA included as a key analytical tool. Through this initiative, both organizations strengthened and accelerated their collaboration to advance high-precision dementia diagnosis.
The Florey, located in Melbourne and recognized as the largest brain research center in the Southern Hemisphere, with more than 500 researchers and staff, is primarily focused on neurodegenerative diseases affecting cognitive function, along with research in depression, schizophrenia, and bipolar disorder.
Professor Peter van Wijngaarden, Executive Director and CEO of the Florey and Honorary Professor of Ophthalmology at the University of Melbourne, has a strong research interest in biomarkers of neurodegenerative diseases. “We are delighted to announce this research collaboration with Neurophet,” said Professor van Wijngaarden. “Through this partnership, we aim to accelerate research toward advanced dementia diagnosis.”
According to DelveInsight’s “Alzheimer’s Disease Diagnostic Market Report”, the global Alzheimer’s disease (AD) diagnostic market will grow at a CAGR of 10.97% during the forecast period from 2024 to 2030. The Alzheimer’s disease (AD) diagnostic market is observing an optimistic market growth due to factors such as a rise in the regulatory approvals for Alzheimer’s disease (AD) diagnostics across the globe. Further, the rising prevalence of head injuries owing to accidents, workplace injuries, and others, and the rise in the geriatric population will increase the prevalence of Alzheimer’s disease, thereby increasing the demand for Alzheimer’s disease diagnostic devices across the globe. Additionally, the increasing research and development of novel biomarkers, the presence of key players in the market, increasing product launches and approvals, and other factors will create a need for Alzheimer’s disease diagnostics in the upcoming years. Therefore, the market for Alzheimer’s disease (AD) diagnostics is estimated to grow at a substantial CAGR during the forecast period from 2024 to 2030.
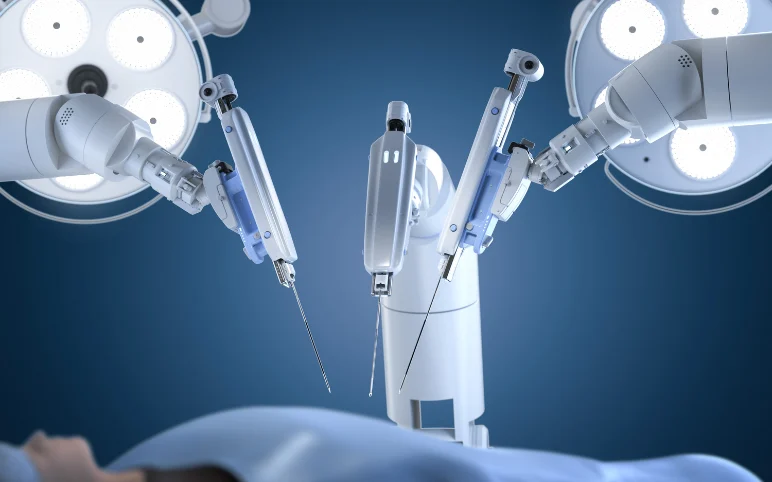
VSI® Performed World’s First Robotic Minimally Invasive Bertolotti’s Resection Surgery
On November 25, 2025, VSI® Spine Surgeon Dr. Christopher Good reached a major milestone in robotic spine surgery when he performed the world’s first minimally invasive robotic Bertolotti’s resection surgery at Reston Hospital Center (HCA Virginia Health System). This groundbreaking procedure introduced a new surgical option for patients with chronic low back pain caused by Bertolotti’s Syndrome an often-overlooked spinal condition affecting roughly 4–8% of individuals.
Historically, surgery for Bertolotti’s Syndrome involved large incisions and significant disruption of soft tissue to reach the deep transitional bone. Dr. Good’s method replaced this extensive exposure with a robotically guided, minimally invasive technique that significantly reduced surgical trauma.
Through advanced preoperative computerized planning, he determined the precise angles and trajectories required for each bone cut before entering the operating room. This planning enabled the robot-assisted procedure to be performed through a single 22-millimeter incision, allowing for accurate removal of the problematic bone while preserving surrounding muscle and soft tissue.
According to DelveInsight’s “Surgical Robotic System Market Report,” the global surgical robotic systems market was valued at USD 11,082.32 million in 2024, growing at a CAGR of 13.21% during the forecast period from 2025 to 2032 to reach USD 29,785.13 million by 2032. The rising incidence of chronic disorders such as cancer, cardiovascular diseases, and orthopedic conditions is significantly boosting the demand for advanced surgical interventions, thereby propelling the growth of the surgical robotic systems market. As chronic conditions often require complex, high-precision surgeries, robotic-assisted procedures offer enhanced accuracy, minimal invasiveness, and quicker recovery times, making them highly suitable for treating such ailments. Simultaneously, the increasing number of surgical procedures globally, driven by an aging population and a higher prevalence of lifestyle-related health issues, is further underscoring the need for efficient and precise surgical tools. In response, key market players are heavily investing in product development activities, focusing on innovations such as compact robotic platforms, AI integration, and enhanced visualization systems. These advancements not only expand the scope of robotic surgery across specialties but also improve surgical outcomes, thereby contributing to the growth of the surgical robotic systems market during the forecast period from 2025 to 2032.
BioWave® Announced New Clinical Data Demonstrating Impactful Non-Invasive Pain Relief for War-Related Injuries and Home-Based Treatments
On November 20, 2025, BioWave® Corp., a leading developer of non-invasive neuromodulation technologies for pain management, reported interim findings from two ongoing studies at the 2025 American Society of Regional Anesthesia and Pain Medicine Annual Meeting in Austin, Texas. The results highlighted once again the strong clinical performance and adaptability of BioWave’s patented high-frequency neuromodulation technology across diverse pain conditions from severe battlefield injuries in Ukraine to chronic pain treated at home.
Working with Imperial College Healthcare in London and the Regional Clinical Hospital of Ivano-Frankivsk in Ukraine, researchers conducted a study involving roughly 50 patients, many of whom had suffered major battlefield injuries, including amputations and nerve trauma.
Using BioWave’s proprietary technology, the study showed pain levels fell from an average of 6.68 to 3.24 immediately after treatment, meaningful pain relief lasted an average of 17.2 hours after a single 30-minute session, patients experienced better comfort, mobility, and easier prosthetic use, with reductions in phantom-limb pain, treatments were tolerated extremely well, with no adverse events and sustained benefits during repeated use.
While acute care for battlefield trauma is often delivered quickly, long-term pain management remained a significant challenge. Many patients continued to face neuropathic and phantom limb pain due to limited medical resources, shortages of specialists, and the realities of an active war zone. These issues delayed rehabilitation and affected mobility, emotional well-being, and overall recovery.
Early use of BioWave’s neuromodulation technology offered a drug-free, safe alternative that could be administered in hospitals, field environments, or at home. By rapidly reducing pain, lowering reliance on long-term medications, and improving function, the therapy helped patients return to rehabilitation sooner and regain a better quality of life.
A second study presented at the ASRA meeting by Arun Kumar Bhaskar¹, Helen Walsh², and Dominic Hegarty³ reviewed more than 10,400 patient-reported outcomes and validated them using public feedback data. Patients had been using BioWave devices at home to manage various chronic pain conditions such as back and sciatica pain (42%), shoulder pain (14%), and neck or headache pain (13%).
The study found pain scores dropped from 7.8 to 3.9. 93% of users reported an improvement in quality of life. 43% reduced or stopped their pain medications. 65% experienced better mood and sleep. 56% reported better sleep quality. 97% indicated they would continue using BioWave therapy long term.
Overall, the findings confirmed that BioWave’s non-invasive neuromodulation technology served as an effective solution for chronic pain management, providing deep, targeted pain relief without surgery or implants. The technology offered a safe, economical option for both clinical practice and home-based care, helping patients reduce medication use, improve mobility, and achieve lasting relief.
According to DelveInsight’s “Neuromodulation Devices Market Report”, the global neuromodulation devices market is expected to increase from USD 7,862.04 million in 2024 to USD 16,111.10 million by 2032, reflecting strong and sustained growth, growing at a CAGR of 9.44% during the forecast period from 2025 to 2032. The market for neuromodulation devices is growing rapidly, fueled by the rising global prevalence of chronic diseases like pain, epilepsy, and depression. This growth is also driven by significant technological advancements that have made devices smaller, smarter, and more effective. Favorable regulatory policies and better reimbursement coverage are also making these treatments more accessible. Overall, the increasing demand for effective, long-term therapeutic options for neurological and chronic conditions is driving a strong, sustained market.