Gastroparesis Treatment: How Nutrition Can Support Symptom Management?
Oct 08, 2025
Table of Contents
Gastroparesis is a digestive condition in which the stomach empties food into the small intestine slower than normal. This delay can cause nausea, bloating, abdominal discomfort, and a feeling of fullness even after eating small meals. Understanding the right gastroparesis diet modification is crucial for managing symptoms, promoting better digestion, and improving quality of life.
Understanding Gastroparesis and Its Symptoms
Common gastroparesis symptoms include early satiety, nausea, vomiting, heartburn, and abdominal pain. These symptoms often worsen after consuming high-fat or high-fiber meals that slow gastric emptying further. While there is no single gastroparesis cure, nutrition and lifestyle adjustments can go a long way toward healing gastroparesis naturally and reducing symptom flare-ups.
Downloads
Click Here To Get the Article in PDF
In many cases, gastroparesis is linked to underlying conditions such as diabetes, thyroid disorders, or nerve damage that affect the stomach’s muscle contractions. However, some people may develop idiopathic gastroparesis, where no clear cause is identified. Stress, medications, and hormonal fluctuations can also aggravate symptoms. Recognizing these triggers is essential to tailor a natural treatment for gastroparesis and identify the most effective gastroparesis diet modification for individual needs. Early diagnosis and lifestyle intervention play a key role in slowing disease progression and supporting natural gastroparesis treatment.
The Role of Diet in Gastroparesis Management
Diet plays a crucial role in managing gastroparesis, a condition in which the stomach empties food more slowly than usual. Proper nutrition can help alleviate symptoms such as nausea, bloating, and early satiety, improving overall quality of life. Tailoring food choices, meal size, and consistency can significantly impact symptom control. Understanding which foods to include and which to avoid is crucial for effective management of gastroparesis. This approach complements medical treatments and can serve as a cornerstone of long-term care.
Foods to Eat When Managing Gastroparesis
When it comes to managing gastroparesis effectively, nutrition plays a pivotal role. A well-planned gastroparesis diet can significantly reduce symptoms, improve digestion, and enhance energy levels. The key principle of gastroparesis diet modification is to choose foods that are easy to digest, low in fat and fiber, and gentle on the stomach. Since gastroparesis slows gastric emptying, meals should be soft, well-cooked, and taken in smaller portions throughout the day.
Low-fat foods are especially beneficial because fat delays stomach emptying and can worsen nausea or bloating. Opting for lean proteins such as skinless chicken, turkey, white fish, tofu, or egg whites helps meet nutritional needs without overburdening the digestive system. Similarly, choosing low-fat dairy products, such as yogurt, cottage cheese, or skim milk, can provide essential nutrients without contributing to delayed digestion.
Soft and pureed foods form another cornerstone of natural treatment for gastroparesis. These include soups, smoothies, mashed potatoes, pureed vegetables, applesauce, and oatmeal. Blending or pureeing foods breaks down their fiber content and makes them easier to digest. Liquid-based meals, such as broths or meal-replacement shakes, often pass through the stomach more easily than solid foods and can help maintain calorie intake when solid meals are difficult to tolerate.
Low-fiber options are equally important in a functional medicine gastroparesis approach. High-fiber foods like raw vegetables, legumes, and whole grains tend to stay in the stomach longer, worsening symptoms or causing bezoar formation. Instead, refined grains such as white rice, white bread, and regular pasta are better tolerated. Peeled and cooked fruits, such as bananas, peaches, or applesauce, can also be safely included in moderation.
Small, frequent meals, typically five to six per day, are highly recommended. Eating smaller portions prevents overfilling the stomach and reduces the risk of nausea, bloating, or pain. Patients can also try separating solids and liquids during meals; for instance, drink fluids at least 30 minutes before or after eating to aid digestion. Warm fluids, such as herbal teas or broths, can further help promote gastric emptying and soothe the stomach lining.
Hydration plays a key role in healing gastroparesis naturally. Sipping on clear liquids such as water, electrolyte drinks, or herbal teas throughout the day keeps digestion flowing smoothly. Including nutrient-dense smoothies made from low-fat yogurt, banana, and a touch of honey can ensure adequate calorie intake and provide gentle nourishment.
Finally, incorporating foods rich in natural digestive aids may further support gastric motility. Ginger, for example, is well known in natural remedies for gastroparesis for its ability to ease nausea and promote stomach emptying. Similarly, peppermint and chamomile teas can relax the digestive tract and alleviate discomfort. Combining these dietary strategies with mindful eating habits, such as eating slowly, chewing thoroughly, and sitting upright after meals, can greatly improve digestive comfort and overall well-being.
By focusing on these dietary principles, individuals can practice holistic treatment for gastroparesis and gradually experience relief through natural treatment for gastroparesis, ultimately regaining control over their digestive health.
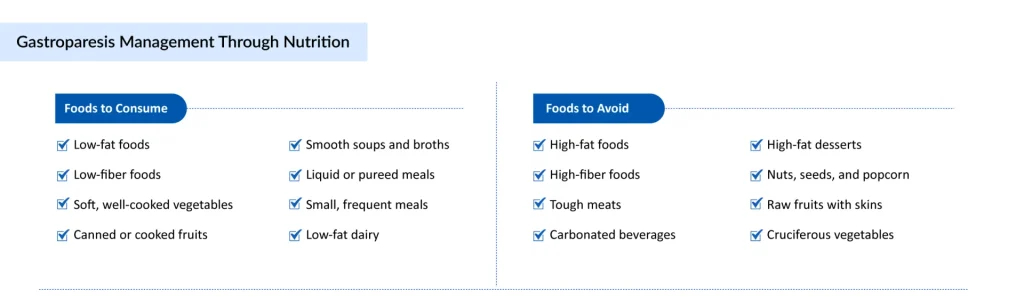
Foods to Avoid in Gastroparesis
Managing gastroparesis symptoms effectively requires careful dietary awareness. Certain foods can slow down stomach emptying, increase bloating, and worsen nausea, making them important to limit or eliminate. A proper understanding of foods to avoid for gastroparesis is an essential part of gastroparesis diet modification and overall natural treatment for gastroparesis. Below are the key food categories that may aggravate symptoms and delay digestion:
High-Fat Foods: Fat naturally slows gastric emptying — a major concern for people with gastroparesis. While healthy fats are important for energy, excessive fat intake can make gastroparesis symptoms worse. Avoid fried foods, fast food, full-fat dairy, creamy sauces, butter, cheese, and fatty meats like bacon, sausage, or pork belly. These foods stay in the stomach for a long time, leading to nausea, bloating, and early fullness. If you need fats in your diet, use small amounts of healthy oils such as olive oil or avocado oil, and incorporate them in pureed or liquid meals. This approach can help speed up gastric emptying naturally while still meeting nutritional needs.
High-Fiber Foods: Fiber, while beneficial for most people, poses a challenge in gastroparesis because it’s harder to digest and can form bezoars (solid masses of undigested food) in the stomach. Foods high in insoluble fiber — such as raw vegetables, whole grains, legumes, nuts, seeds, and fruit skins — can worsen symptoms like abdominal pain and bloating. Avoid foods such as broccoli, cauliflower, beans, lentils, corn, apples with skin, and bran cereals. Instead, choose low-fiber options like refined grains, peeled fruits (such as peaches or pears), and well-cooked or pureed vegetables. This adjustment is a vital step in functional medicine for gastroparesis, which emphasizes individualized nutrition for better digestion.
Carbonated Beverages and Alcohol: Carbonated drinks like soda, sparkling water, and beer can trap gas in the stomach, leading to painful bloating and fullness. Alcohol, especially in large amounts, can irritate the stomach lining and further slow motility. For gastroparesis self-care, replace carbonated beverages with still water, herbal teas (ginger or chamomile are great herbal remedies for gastroparesis), or electrolyte-rich drinks. These can help promote gastric emptying and hydration without adding gas or acidity.
High-Fat Desserts and Sugary Foods: Desserts like pastries, doughnuts, chocolate, and ice cream often combine fat and sugar, both of which delay digestion. Excess sugar can also cause blood sugar spikes, particularly in diabetic gastroparesis, making symptoms worse. Choose naturally sweet options such as fruit purees, gelatin-based desserts, or low-fat yogurt. This change supports natural remedies for gastroparesis and helps maintain energy levels without aggravating the digestive system.
Tough Meats and Fibrous Foods: Dense meats such as steak, lamb, or pork require strong stomach contractions for digestion — something that’s impaired in gastroparesis. Similarly, fibrous foods like raw carrots, celery, pineapple, and corn are slow to break down. Opt for tender, well-cooked meats that are shredded or minced. Soft proteins like eggs, tofu, or fish digest more easily and align with natural gastroparesis treatment principles that emphasize gentle, nutrient-rich foods.
Dairy Products (for Sensitive Individuals): While low-fat dairy can be part of a gastroparesis diet, some individuals experience lactose intolerance, which can worsen bloating and discomfort. If dairy triggers your symptoms, consider lactose-free milk, almond milk, or oat milk as alternatives. This modification supports holistic treatment for gastroparesis, reducing inflammation and digestive strain.
Raw Fruits and Vegetables: Raw produce like salads, kale, apples, oranges, and bell peppers can be difficult to digest in gastroparesis due to their fiber content and texture. Cooking, peeling, or pureeing these foods helps break down their fibers, making them easier on the stomach. Soups and vegetable purees can be excellent options in natural treatments for gastroparesis, providing nutrients without adding digestive stress.
Avoiding these triggers can help in how to speed up gastric emptying naturally and reduce discomfort after meals.
Natural, Holistic, and Home-Based Approaches to Gastroparesis Management
Managing gastroparesis effectively often involves more than dietary changes; incorporating natural remedies for gastroparesis and holistic practices can provide additional relief. Herbal options, such as ginger, peppermint, and chamomile, can soothe the stomach and improve motility, while probiotics support gut health. Mind-body practices, including gentle yoga and acupuncture, help reduce stress and enhance digestive function, reflecting holistic treatment for gastroparesis principles. At home, simple self-care habits, such as eating smaller, more frequent meals, chewing food thoroughly, drinking warm fluids, staying hydrated, and avoiding lying down immediately after eating, can significantly improve symptoms. Light physical activity after meals can also help promote gastric emptying naturally. Combining these approaches with gastroparesis home remedies empowers patients to manage symptoms, support digestion, and complement conventional gastroparesis treatments, providing a more comprehensive path to healing gastroparesis naturally.
Conclusion
Managing gastroparesis effectively requires a combination of careful dietary planning, lifestyle adjustments, and natural remedies. By following a tailored gastroparesis diet that focuses on easily digestible, low-fat, and low-fiber foods and avoiding known triggers, patients can significantly reduce discomfort and improve gastric motility. Small, frequent meals, proper hydration, and mindful eating habits form the cornerstone of gastroparesis self-care, contributing to better symptom management.
In addition to dietary strategies, natural treatments for gastroparesis, such as herbal remedies, probiotics, gentle exercise, and stress-reducing practices, can complement conventional gastroparesis treatment approaches. While there is currently no definitive gastroparesis cure, adopting these holistic methods, exploring alternative treatments for gastroparesis, and maintaining consistent medical guidance can help individuals heal gastroparesis naturally, enhance digestion, and improve overall quality of life.

FAQs
Nutrition interventions are planned actions aimed at improving an individual’s nutritional status and overall health. They may involve changes in diet, supplementation, education, or therapeutic approaches to prevent or manage malnutrition, chronic diseases, or specific nutrient deficiencies.
While nutrition interventions cannot reverse cirrhosis caused by chronic liver disease, they can play a preventive role in the early stages of liver damage. A balanced diet, reduced alcohol intake, adequate protein, and micronutrient support can help prevent further liver injury, reduce complications, and improve liver function in individuals at risk.
Resetting your diet and wellness through nutrition intervention involves a comprehensive approach. It begins with assessing your current nutritional status and eating habits to identify areas for improvement. This is followed by eliminating processed foods, excess sugar, and unhealthy fats, while emphasizing whole foods such as fruits, vegetables, lean proteins, and healthy fats. Key lifestyle practices, including proper hydration, portion control, and regular physical activity, are integrated to support overall well-being. Additionally, targeted nutrition interventions, such as meal planning, supplementation, or the use of functional foods, are employed to address deficiencies and optimize health.
The most effective interventions for addressing inadequate nutrition vary depending on the severity and underlying cause, but generally encompass several key strategies. Nutrition counseling is often the first step, offering personalized dietary guidance tailored to individual needs. Oral nutritional supplements can provide additional calories, protein, and essential micronutrients to support overall health. In some cases, fortified foods or specialized therapeutic diets are recommended to enhance nutrient intake. For severe cases where oral intake is insufficient, enteral or parenteral nutrition may be necessary to ensure adequate nourishment and prevent further complications.
After a bowel resection, early nutrition intervention is critical because the body’s nutrient absorption is compromised, leading to potential deficiencies. Providing adequate protein, vitamins, and minerals supports healing and recovery while preventing malnutrition, muscle loss, and post-operative complications. Implementing early enteral feeding or carefully tailored diets also helps restore gut function, ultimately improving overall patient outcomes.
While gastroparesis may not be fully “cured” through natural methods, its symptoms can be effectively managed with certain lifestyle and dietary strategies. Patients are encouraged to eat small, frequent meals that are low in fat and fiber, and to choose easily digestible foods such as smoothies, soups, or purees. Staying well-hydrated while avoiding carbonated drinks can also help ease digestive discomfort. Additionally, incorporating gentle physical activity can stimulate digestion, and working with a dietitian can provide personalized meal planning tailored to individual needs.
The three main types of nutrition interventions include nutrition-specific, nutrition-sensitive, and behavior change interventions. Nutrition-specific interventions directly target nutritional deficiencies through measures such as supplementation and therapeutic feeding. Nutrition-sensitive interventions focus on addressing the underlying causes of malnutrition, including poverty and food insecurity, through initiatives like agricultural programs and social protection schemes. Behavior change interventions aim to promote healthy eating habits and lifestyle practices, typically through nutrition education and counseling.
Nutrition-specific interventions are direct actions aimed at addressing nutrient intake and status. Ten examples include Breastfeeding promotion and support, Complementary feeding programs for infants and toddlers, Micronutrient supplementation (iron, vitamin A, iodine, zinc), Therapeutic feeding for severe acute malnutrition, Fortification of staple foods with essential vitamins and minerals, Oral nutritional supplements for at-risk populations, Management of maternal nutrition during pregnancy and lactation, Treatment of moderate malnutrition with fortified foods, School-based nutrition programs, and Counseling for dietary diversity and balanced nutrition.



