Chronic Venous Insufficiency Treatment: Bridging Unmet Needs with Minimally Invasive and Regenerative Solutions
Jan 19, 2026
Table of Contents
Summary
- In the seven major markets (7MM: US, EU4, UK, Japan), diagnosed cases of CVI reached ~17 million in 2024. Prevalence is projected to grow at a 1.4% CAGR, reaching ~20 million by 2034, driven by aging populations, obesity, sedentary lifestyles, and improved diagnostics.
- Endovenous laser ablation (EVLA) and radiofrequency ablation (RFA) are now first-line interventional options, offering high success rates, minimal invasiveness, and rapid recovery.
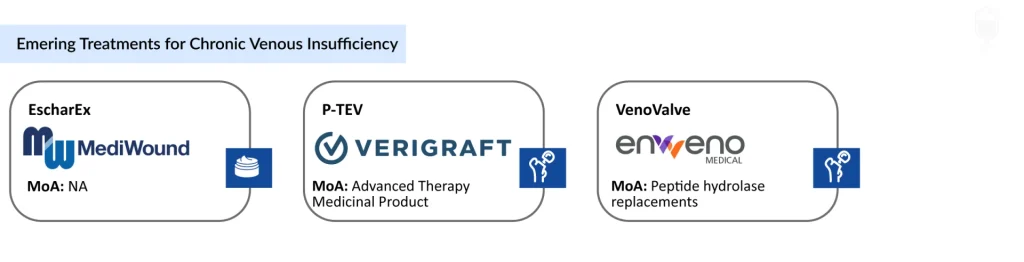
- Device-based therapies include enVVeno’s VenoValve, a bioprosthetic venous valve with FDA Breakthrough Device Designation, and the less invasive EnVVe transcatheter system.
- Theraclion’s SONOVEIN uses non-invasive high-intensity focused ultrasound (HIFU) to ablate veins without surgery or anesthesia.
- Regenerative therapies such as VERIGRAFT’s Personalized Tissue-Engineered Vein (P-TEV) aim to restore venous function using bioengineered grafts.
- Wound-care innovations, including MediWound’s EscharEx, support faster healing of venous leg ulcers through non-surgical debridement.
Chronic venous insufficiency (CVI) represents a significant burden in vascular medicine, affecting millions worldwide with symptoms ranging from leg swelling to severe ulcers. The chronic venous insufficiency treatment landscape combines conservative measures, pharmacotherapy, and advanced interventions, evolving toward minimally invasive options and novel pipeline therapies.
Downloads
Click Here To Get the Article in PDF
CVI arises from damaged venous valves in the legs, causing blood to pool and leading to venous hypertension. Classified by the CEAP system (C0 to C6), it progresses from asymptomatic varicose veins (C2) to active ulcers (C6), with higher prevalence in women (57%) and older adults. In the seven major markets (7MM: US, EU4, UK, Japan), diagnosed CVI prevalent cases reached 17 million in 2024, projected to grow at 1.4% CAGR to 20 million by 2034, driven by aging populations and better diagnostics. With rising life expectancy, increasing obesity rates, sedentary lifestyles, and improved diagnostic awareness, the prevalence of CVI continues to grow.
Chronic Venous Insufficiency Treatment: Conservative Management and Lifestyle Interventions
The primary objectives of CVI treatment include reducing venous hypertension, relieving symptoms, preventing disease progression, promoting ulcer healing, minimizing recurrence, and improving overall functional outcomes. As a result, CVI management typically follows a stepwise and multimodal approach, escalating from conservative therapies to interventional or surgical strategies as disease severity increases.
Compression Therapy: Foundation of Care
Compression therapy remains the cornerstone of CVI management across all stages of disease. Modalities include graded compression stockings, multilayer bandaging systems, and intermittent pneumatic compression devices. By exerting external pressure on the lower extremities, compression therapy reduces venous distension, enhances venous return, improves valve competence, and mitigates edema.
Extensive clinical evidence supports the effectiveness of compression therapy in alleviating symptoms, slowing disease progression, and improving venous ulcer healing rates. Despite its proven benefits, long-term adherence remains a major challenge due to discomfort, difficulty of use, aesthetic concerns, and inadequate patient education. Improving compliance remains a critical focus in real-world CVI management.
Pharmacological Therapies
Pharmacological treatment in CVI is primarily aimed at symptom control, improving microcirculatory function, and reducing inflammation rather than correcting the underlying venous anatomy.

Venoactive Drugs (VADs)
Venoactive drugs are widely used in the management of CVI, particularly in Europe and other international markets. These agents act by improving venous tone, reducing capillary permeability, enhancing lymphatic drainage, and exerting anti-inflammatory effects. Commonly prescribed VADs include micronized purified flavonoid fraction (MPFF), oxerutins, rutosides, and plant-derived extracts such as horse chestnut seed extract.
MPFF is among the most extensively studied agents in this class and has demonstrated benefits in reducing leg pain, heaviness, edema, and accelerating venous ulcer healing when used alongside compression therapy. However, heterogeneity in clinical guidelines, regulatory approvals, and reimbursement policies continues to influence their adoption across geographies.
Adjunctive Medications
Additional pharmacological agents are used selectively based on individual patient needs. Diuretics may be prescribed for short-term management of edema, pentoxifylline is sometimes used to enhance venous ulcer healing, and anticoagulants are indicated in patients with coexisting thrombotic risk. These therapies are typically supportive and not intended as long-term standalone solutions.
Minimally Invasive Interventional Procedures
Minimally invasive endovenous therapies have reshaped the CVI treatment paradigm and are now considered first-line interventional options for many symptomatic patients.
Endovenous Laser Ablation (EVLA)
EVLA involves ultrasound-guided insertion of a laser fiber into the incompetent vein. Laser energy induces thermal injury to the vein wall, resulting in fibrosis and permanent vein closure. EVLA is associated with high procedural success rates, minimal invasiveness, and rapid post-procedure recovery.
Radiofrequency Ablation (RFA)
RFA uses radiofrequency energy delivered via a catheter to generate controlled thermal damage, leading to vein collapse and occlusion. Clinical outcomes with RFA are comparable to EVLA, with some studies suggesting reduced post-procedural pain and bruising.
Sclerotherapy
Sclerotherapy involves injecting a liquid or foam sclerosant into the affected vein, causing endothelial damage and subsequent vein obliteration. It is commonly used for small varicose veins and reticular veins, and as an adjunct to EVLA or RFA. Compression therapy is routinely recommended following treatment to optimize outcomes.
The growing preference for these minimally invasive approaches reflects their favorable safety profiles, outpatient feasibility, and improved patient satisfaction compared to traditional surgery.
Surgical Treatment Approaches
Surgical intervention remains relevant for a subset of CVI patients, particularly those with advanced disease, complex venous anatomy, or failure of endovenous therapies.
High Ligation and Vein Stripping
High ligation and stripping involve surgical ligation and removal of incompetent superficial veins. While effective, these procedures are associated with longer recovery periods, increased postoperative discomfort, and higher complication rates, which have led to declining utilization in favor of less invasive techniques.
Venous Reconstruction and Bypass
In cases of severe deep venous insufficiency or obstruction, venous bypass or reconstructive surgery may be considered. These procedures are technically demanding and reserved for carefully selected patients managed at specialized centers.
Emerging Innovations Reshaping the CVI Treatment Landscape
The CVI treatment landscape is witnessing renewed innovation, particularly aimed at addressing unmet needs in deep venous disease and advanced-stage CVI.
Device-Based Innovations
enVVeno Medical Corporation is developing the VenoValve, a surgically implanted bioprosthetic venous valve designed to restore unidirectional blood flow in patients with deep venous CVI. The device has received FDA Breakthrough Device Designation and Investigational Device Exemption (IDE) approval, highlighting its potential to transform the management of deep venous insufficiency. A transcatheter-based venous valve replacement system (EnVVe) is also under development, offering a less invasive alternative.
Theraclion’s SONOVEIN platform represents another novel approach, utilizing high-intensity focused ultrasound (HIFU) to ablate veins non-invasively without incisions, catheters, or anesthesia.
Regenerative and Biologic Therapies
VERIGRAFT’s Personalized Tissue-Engineered Vein (P-TEV) is an advanced CVI therapy medicinal product designed to serve as a bioengineered vascular graft. By combining decellularized allogeneic vein scaffolds with autologous patient blood components, P-TEV aims to deliver durable venous reconstruction without immunosuppression. Early clinical studies have demonstrated encouraging safety and patency outcomes.
Innovations in Wound Care
For patients with CVI-associated venous leg ulcers, therapies targeting wound healing are gaining prominence. MediWound’s EscharEx, a bromelain-based enzymatic debridement therapy, selectively removes necrotic tissue and biofilm while preserving viable tissue. This non-surgical approach has the potential to accelerate wound healing and reduce the need for surgical debridement in high-risk patients.
Future CVI Treatment Outlook Looks Promising
The CVI treatment landscape is expected to shift toward earlier diagnosis, personalized therapy selection, and broader adoption of innovative device-based and regenerative solutions. Advances in imaging technologies, digital health tools, and remote patient monitoring may further enhance disease management and long-term outcomes.
In the 7MM, the US had the largest market for chronic venous insufficiency in 2023. The total market size in the US for chronic venous insufficiency was estimated at nearly USD 1.2 billion in 2023 and is expected to grow during the forecast period (2025–2034). By 2034, among all the treatments, the highest revenue is expected to be generated by Laser Ablation/Radiofrequency Ablation, i.e., USD 1.7 billion, while the lowest revenue is expected to be generated by TR987, i.e., USD 20.3 million in the 7MM.
The future outlook for chronic venous insufficiency (CVI) treatment looks increasingly promising as advances in medical technology, pharmacotherapy, and minimally invasive procedures converge to offer safer, more effective, and patient-friendly options. Innovations such as improved endovenous ablation techniques, including laser, radiofrequency, and mechanochemical approaches, continue to refine outcomes with faster recovery and lower complication rates. At the same time, next-generation compression therapies and wound-care products are enhancing quality of life for patients struggling with edema and ulceration, while emerging biologic agents that target underlying venous inflammation and remodeling hold potential to alter disease progression rather than just relieve symptoms.
In parallel with procedural and device improvements, a growing understanding of the molecular and genetic drivers of venous disease is opening doors to targeted pharmacologic treatments aimed at improving venous tone, reducing pathological reflux, and modulating extracellular matrix changes in the venous wall. Digital health tools and remote monitoring are also empowering patients and clinicians to better track symptoms and tailor interventions over time. Taken together, these developments suggest a future in which CVI management becomes more personalized, less invasive, and more effective at preventing long-term disability, offering real hope to millions affected by this chronic condition.