New Horizons in Cocaine Use Disorder (CUD) Treatment Space
Jul 31, 2023
Table of Contents
Cocaine use disorder also known as cocaine dependence is a chronic condition that affects millions of people worldwide. Cocaine is a highly addictive central nervous system stimulant derived from the leaves of the coca plant and produces a range of effects on the mind and body, including short-lived euphoria, increased energy, and alertness that is followed by a crash and intense cravings that often lead to repeated usage.
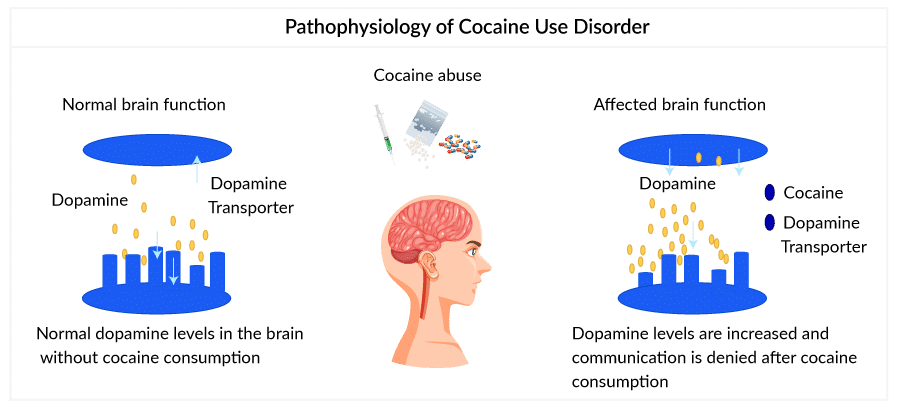
Cocaine use increases the natural chemical messenger dopamine in the brain circuits that control movement and reward. Cocaine prevents dopamine from being recycled and causes a large amount to build up in the space between nerve cells, stopping normal communication. This flood of dopamine in the brain reward circuit strongly reinforces drug-consuming behaviors. As a result of regular cocaine consumption, the reward circuit becomes less sensitive and the person takes stronger and more frequent doses to feel the same high and relieve withdrawal.
Downloads
Click Here To Get the Article in PDF
Despite the risks, cocaine continues to be a popular drug of abuse among youngsters and adults and has been linked to a range of negative health outcomes, including heart attacks, strokes, and mental health disorders. Symptoms of a cocaine use disorder, include agitation, paranoia, hallucinations, delusions, violence, as well as suicidal and homicidal thinking. Cocaine use disorder is diagnosed as a mental health disorder and is classified as a substance use disorder (SUD) in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
Current Cocaine Use Disorder Treatment Landscape: A Blend of Behavioral and Off-label Therapies
Current cocaine use disorder treatment focuses on behavioral therapies, such as cognitive behavioral therapy (CBT), contingency management, and motivational interviewing that can help individuals learn new coping skills to manage drug cravings and other triggers. CBT helps individuals identify and challenge negative thought patterns and behaviors, while contingency management involves providing rewards or incentives for abstaining from drug use. Motivational interviewing is a patient-centered approach that helps individuals increase motivation and self-efficacy for change.
Pharmacotherapy, or the use of medications to treat addiction, has been effective in reducing drug cravings and preventing relapse. Due to a lack of FDA-approved medications for cocaine use disorder treatment, off-label therapies such as antidepressants (bupropion, desipramine, etc.), anti-seizure medications (such as topiramate), and dopamine agonists (modafinil, disulfiram, etc.) are widely used. Antidepressants block the reuptake of catecholamines that stabilizes receptors and are used for symptom withdrawal of chronic cocaine abuse. Further, modafinil a dopamine agonist increases dopaminergic neurotransmission by blocking the dopamine transporter. It also enhances glutamate neurotransmission, increases dopamine transmission, or ameliorates the glutamate depletion seen in chronic cocaine users.
These cocaine use disorder medications have shown positive results such as reduced drug cravings and improved cocaine use disorder symptoms (mood and anxiety). However, more research is needed to determine their long-term effectiveness and safety.
The cocaine use disorder treatment requires a tailored approach that addresses the individual’s unique needs and challenges. Addiction, being a complex brain disorder requires a combination of behavioral therapy, pharmacotherapy, and innovative approaches, to successfully treat the disorder and improve patient outcomes.
There are a number of organizations, such as The National Institute on Drug Abuse (NIDA), Substance Abuse and Mental Health Services Administration (SAMHSA) in the US, and The National Institute for Health and Care Excellence (NICE) in the UK that are dedicated to helping individuals overcome addiction to cocaine and other drugs. These organizations provide a range of services, including education, counseling, and support to individuals and their families.
Advancements in the Management of Cocaine Use Disorder
DEPI Platform: DEPI is the first precision medicine platform for patients with neurodevelopmental disorders (NDDs), and neuropsychiatric disorders. The precision medicine approach begins with ‘endophenotyping’— identifying the nonbehavioral physical and molecular presentations of NDDs and characterizing subgroups of patients with similar disease signatures. DEPI matches these patient subgroups with an NDD-targeted drug (or drug combination) by integrating and analyzing large omics data sets, including genomics, proteomics, pharmacogenomics, and clinical data. The DEPI platform has been validated in a clinical setting showing high specificity, sensitivity, and positive predictive value in prospectively designed trials recalling ‘high’ responder patients to previously failed drug candidates.
- Stress relievers: Studies have shown that individuals with a history of trauma or chronic stress may be more susceptible to developing cocaine use disorder and that exposure to stress can increase the risk of relapse in individuals in recovery. Drugs that block stress-induced relapse are being explored as a potential treatment for cocaine and other drug use disorders
- Pharmacogenetic approaches: Genetic and epigenetic factors have been found to play a role in the development of cocaine use disorder. Certain genetic variations may make individuals more vulnerable to addiction, while epigenetic changes can alter the expression of genes involved in the brain’s reward system and increase the risk of addiction. The aim of pharmacogenetics is to identify effective ‘personal therapies’ based on the genetic individual background to ensure greater effectiveness
- Transcranial magnetic stimulation (TMS): It is a non-invasive brain stimulation technique that stimulates specific regions of the brain and provides insights into the neural networks affected by cocaine use disorder. It is a procedure that uses magnetic fields to stimulate nerve cells in the brain to improve symptoms. It’s called a noninvasive procedure as it is done without using surgery or cutting the skin.
- Neurotransmitters: Latest studies have focused on developing novel medications that can target specific neurotransmitters like gamma-aminobutyric acid (GABA) and glutamate that play a crucial role in the development of cocaine use disorder, while several emerging drugs are being studied for their potential to target these neurotransmitter systems and explore more.
- Vaccine: Vaccines that target cocaine are also being developed and tested in clinical trials, these vaccines work by generating antibodies that bind to cocaine molecules and prevent them from crossing the blood-brain barrier, reducing the drug’s psychoactive effects.
Need of the Moment
- Complex pathophysiology: The pathophysiology of cocaine use disorder is complex and multifactorial, involving a range of biological, psychological, and social factors. Understanding these underlying mechanisms is critical for developing effective treatments for addiction and improving outcomes. Further, cocaine has diverse effects on the brain and involves multiple kinds of neurotransmitters. Thus, unlike the treatment of nicotine and opiate disorders, the pharmacotherapeutic treatments for cocaine use disorder remain challenging and must be directed toward more than one molecular target.
- Limited biomarkers: Despite the diversity of the literature on brain and biological changes related to chronic cocaine use, only a few biomarkers have been identified; definitive biomarkers can help accurately diagnose dependence among a large portion of the population. The prevention and treatment of substance use disorder, including cocaine addiction, will benefit from having better biomarkers, that help classify patients into reproducible categories with predictive validity.
- Lack of approved therapies: Despite being associated with significant mortality, the treatment of cocaine dependence remains devoid of any approved therapy compared with the treatment of other addictive disorders.
- Pithole in the current cocaine use disorder treatment: Despite progress in developing psychosocial cocaine use disorder treatments, many patients still do not respond to current treatments, have high dropout rates, and do not attain substantial periods of cocaine abstinence. Further, current cocaine use disorder treatments are time-consuming, not universally accessible, and suffer low treatment retention.
- Preventing relapse: One of the major unmet needs in cocaine use disorder treatment is the lack of effective medications that can prevent relapse. Although behavioral therapies and pharmacological interventions can reduce drug use and cravings, still the risk of relapse remains high.
- Breaking the taboo: The stigma around substance use in its various forms acts as a barrier to treatment. Policy-makers are not inclined to allot resources and healthcare providers, to effectively screen and treat. Stigma is a problem across health conditions ranging from cancer and HIV to many mental illnesses (borderline personality disorder, obsessive-compulsive disorder, etc.). People with addiction are still blamed for their disease. Hence, stigma plays a key role in treatment-seeking delays, as it decreases the likelihood that a psychiatric patient would seek treatment.
Emerging Therapies: A Ray of Hope for Cocaine Use Disorder Patients
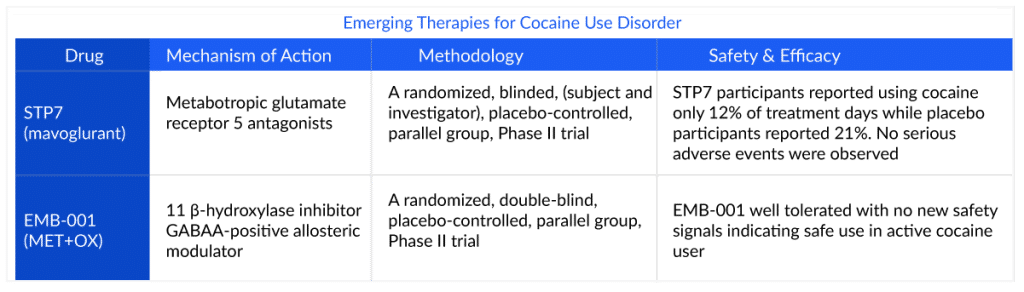
After decades of research and development, novel drugs such as EMB-001 and STP7 (mavoglurant) have shown positive results in clinical trials with the potential to provide longer abstinence and prevent relapse. STALICIA’s STP7 (mavoglurant) is a selective nonallosteric metabotropic glutamate receptor 5 (mGluR5) antagonist which in its Phase II trial has successfully allowed cocaine users to abstain without any withdrawal symptoms or serious adverse events. mGluR5 has been associated with mood disorders, addiction, and rare and common forms of autism. The product is believed to block a certain protein in the brain, which is related to cravings to use drugs like cocaine.
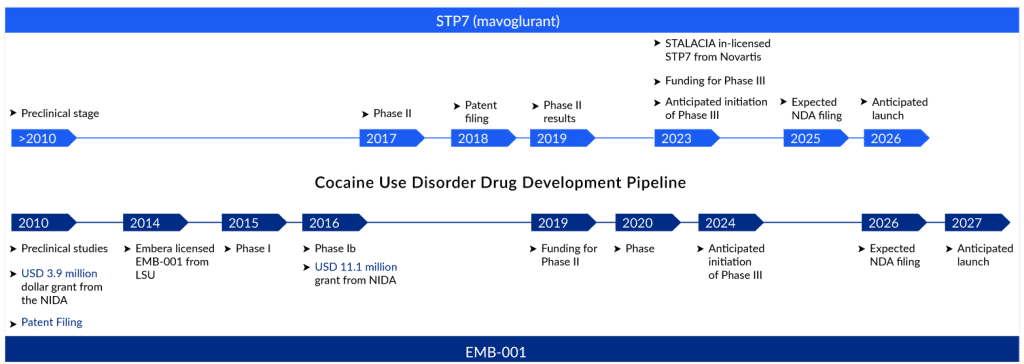
Additionally, the company will be using its precision medicine technology “DEPI” to identify subgroups of high-responder patients. Precision medicine can optimize efficiency or therapeutic benefit for particular groups of patients, especially by applying genetic or molecular characteristics. Hence, if approved, the drug would be the first in the market (2026) and is estimated to generate more than USD 6 million in the US according to Delveinsight’s “Cocaine use Disorder Market” report.
EMB-001 of Embera NeuroTherapeutics is a combination product of the cortisol synthesis inhibitor metyrapone (MET) and the benzodiazepine oxazepam (OX) with the potential to address the significant unmet need for medications to treat and prevent cocaine use disorder. By minimizing the occurrence of relapse, the drug aims to provide long-term abstinence. The unique mechanism of action of EMB-001 targets two different pathways of the stress response, 11 β-hydroxylase inhibitors, and GABAA positive allosteric modulator, hence alleviating relapse. However, the drug targets a smaller patient pool with moderate-severe cocaine use disorder cases; hence generating a lower revenue compared to STP7, and is estimated to attain its peak sales in its 8th year with medium uptake.
Further, in preclinical studies, ALDH2 inhibition has been found to reduce self-administration, cue- and drug-primed relapse in nicotine, alcohol, cocaine, heroin, methamphetamine, and binge eating models and also demonstrated anti-anxiety properties in models of stress. ALDH2 inhibitor technology is being developed by Amygdala Neurosciences and has the potential to prevent drug-seeking behavior, craving, and relapse.
Organizations like The National Institute on Drug Abuse of the National Institutes of Health (NIDA) support the medication development pipeline for treating cocaine use disorder.
Glutamatergic and GABAergic systems seem to be a promising potential new avenue for the treatment of cocaine use disorder. It is still in its early stages, and more research is required to fully understand the efficacy and safety of these emerging therapies.
-Key Opinion Leader
Cocaine dependence and other addictions continue to be global unmet medical needs resulting in significant healthcare burdens and productivity losses. Nevertheless, recent advancements have led to the emergence of effective pharmacotherapies and innovative approaches like precision medicine. The thirst for approved therapy has made the cocaine use disorder treatment market a compelling economy for pharma players, providing an upper hand to the one entering first. Though the emerging cocaine use disorder pipeline is scarce, there is a window of opportunity for bigger pharma players to conduct trials evaluating safer and more effective therapies, and capitalize on an untapped cocaine use disorder treatment market. According to DelveInsight’s estimates, the total size of the seven major cocaine use disorder markets (the United States, Germany, France, Italy, Spain, the United Kingdom, and Japan) is likely to cross the USD 400 million mark by 2032 owing to the launch of emerging therapies, increased awareness, and improved diagnosis.
FAQs
Cocaine use disorder has a catastrophic impact on both people and society. Cocaine use disorder is the obsessive use of cocaine despite the physiological, psychological, and behavioral effects. It is a serious public health issue that affects millions of individuals worldwide.
Symptoms of a cocaine use disorder, include agitation, paranoia, hallucinations, delusions, violence, as well as suicidal and homicidal thinking.
Cocaine use disorder is diagnosed as a mental health disorder and is classified as a substance use disorder (SUD) in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
There is presently no approved medication for cocaine use disorder treatment; psychosocial treatment is the standard. Several psychological treatments are successful, including group counseling, individual drug counseling, cognitive behavioral therapy (CBT), and contingency management; nevertheless, many individuals do not respond to these cocaine use disorder treatments and have significant dropout rates.

Downloads
Article in PDF