The Unmet Needs in Glaucoma Treatment: Bridging Gaps for Better Vision Care
Apr 12, 2024
Table of Contents
Glaucoma, often dubbed as the “silent thief of sight,” poses a significant challenge in the domain of ophthalmology. Glaucoma treatment has made significant strides, yet several unmet needs persist, posing challenges to effective management and vision preservation. By prioritizing early detection, embracing personalized approaches, exploring novel therapeutic targets, advancing surgical innovations, enhancing patient education and adherence, and fostering collaborative care models, we can bridge these gaps and pave the way for improved outcomes in glaucoma management. Only through concerted efforts and innovative solutions can we safeguard the precious gift of sight for millions affected by this insidious disease.
Early Detection and Diagnosis: The Cornerstone of Effective Glaucoma Management
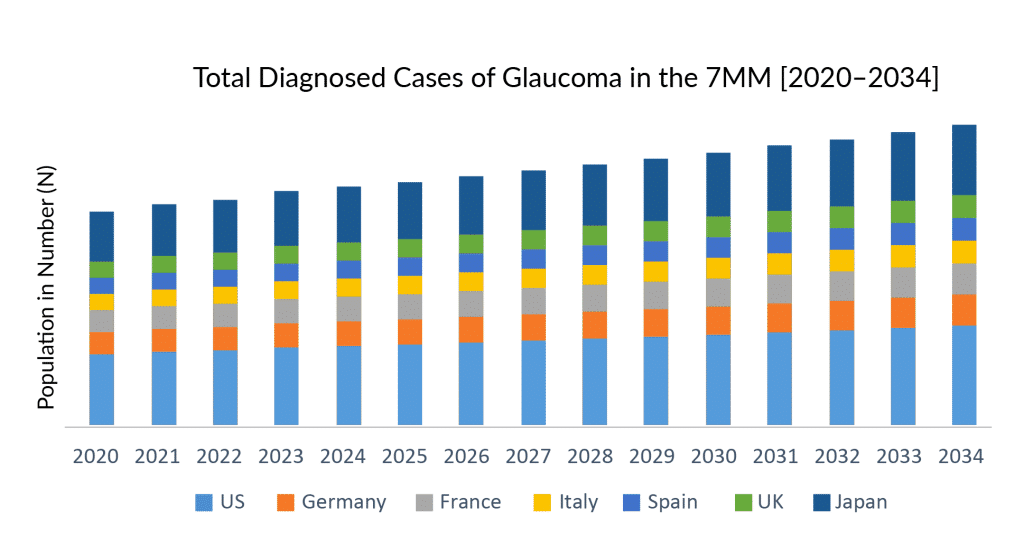
Glaucoma remains undetected in most of the patients due to many factors. According to DelveInsight estimations, of 16 million glaucoma prevalent cases in 2022 in the 7MM, only 7 million cases are estimated to have received a formal diagnosis. As per DelveInsight’s estimates, the US alone accounts for nearly 35% of total diagnosed prevalent cases, for glaucoma in the 7MM, followed by Japan, contributing 23% of all the glaucoma cases.
Downloads
Click Here To Get the Article in PDF
Recent Articles
- Analyzing the Most Promising Drugs That Will Lose Patent in the US & EU in 2022
- Global Top Players in Intraocular Lens (IOL) Market
- Prominent Players in Glaucoma Drainage Devices Market
- Enovis Acquires Novastep; Rockwell Medical Announced Collaboration with B. Braun; Dexcom G7 Recei...
- How Pharmaceutical Companies Are Mitigating The Gap In The Eye Disorders Treatment Market
Early detection and diagnosis stand as the bedrock of effective glaucoma management, offering a vital shield against the progression of this sight-threatening disease. By catching glaucoma in its incipient stages, healthcare providers can institute timely interventions that significantly slow its advancement. Regular eye screenings, especially for individuals at higher risk, such as those with a family history of glaucoma or older adults, become paramount.
Through sophisticated diagnostic tools like tonometry, visual field testing, and optical coherence tomography, practitioners can pinpoint even subtle changes in optic nerve health and intraocular pressure. Armed with these insights, personalized treatment plans can be tailored, whether through medicated eye drops, laser therapy, or surgical procedures, ultimately safeguarding precious vision.
Moreover, the impact of early detection extends beyond individual patients, resonating throughout healthcare systems. By reducing the burden of advanced glaucoma cases requiring intensive treatments, resources can be allocated more efficiently. The societal benefits ripple outward, as preserved vision translates into enhanced quality of life and sustained productivity for those affected.
Educational campaigns advocating regular eye check-ups and awareness of glaucoma’s silent progression further fortify the foundation of early intervention. Through these concerted efforts, the trajectory of glaucoma transforms from a potential blinder to a manageable condition, illuminating a path toward a brighter, clearer future for all those at risk.
Personalized Glaucoma Treatment Approaches: Moving Beyond One-Size-Fits-All
Personalized glaucoma treatment approaches mark a pivotal shift from the traditional one-size-fits-all model, heralding a new era of precision medicine in ophthalmology. With advancements in diagnostic technologies and a deeper understanding of the disease’s multifaceted nature, clinicians now tailor treatments to each patient’s unique characteristics. From genetic predispositions to lifestyle factors, a comprehensive profile informs these customized strategies. This nuanced approach enhances efficacy and minimizes adverse effects, optimizing the patient’s quality of life while combating the progressive vision loss characteristic of glaucoma.
By embracing personalized glaucoma treatment modalities, clinicians can delve into the nuanced landscape of glaucoma subtypes, acknowledging that what works for one patient may not benefit another. Tailored therapies consider factors such as intraocular pressure variations, optic nerve health, and individual medication responses. Through this lens, glaucoma treatment becomes more than just a prescription—it becomes a holistic partnership between patient and practitioner, navigating the intricate terrain of glaucoma management. As research continues to unveil the complexities of this condition, personalized approaches stand as a beacon of hope, promising more effective, targeted, and sustainable solutions for those affected by this sight-threatening disease.
Minimally Invasive Surgical Innovations: Redefining Glaucoma Management
Minimally invasive surgical innovations are revolutionizing the landscape of glaucoma management, offering patients and clinicians alike a promising alternative to traditional invasive procedures. By employing innovative techniques such as micro-incisional glaucoma surgery (MIGS), these procedures aim to mitigate intraocular pressure and halt disease progression with reduced trauma to the eye. Through smaller incisions and advanced instrumentation, MIGS procedures typically entail shorter recovery times and lower complication rates compared to conventional surgeries, thus enhancing patient outcomes and satisfaction.
Moreover, the advent of minimally invasive surgical innovations has ushered in a new era of personalized glaucoma care. Tailored glaucoma treatment plans leveraging MIGS techniques allow ophthalmologists to address varying degrees of disease severity while optimizing patient comfort and visual outcomes. As these innovations continue to evolve, the prospect of achieving long-term glaucoma management with minimal disruption to patients’ daily lives becomes increasingly tangible, promising a brighter future for individuals living with this sight-threatening condition.
Patient Adherence and Education: Bridging the Gap in Glaucoma Treatment
Patient adherence and education are pivotal in bridging the gap in effective glaucoma treatment. Glaucoma, a chronic condition characterized by progressive vision loss, demands consistent adherence to prescribed medications and lifestyle adjustments. Educating patients about the nature of the disease, its implications, and the importance of treatment adherence empowers them to take charge of their eye health. When patients understand the irreversible consequences of untreated glaucoma, they are more likely to adhere to medication schedules and attend regular eye examinations, crucial for disease monitoring. Moreover, tailored education that considers patients’ cultural backgrounds, literacy levels, and personal circumstances fosters a stronger patient-provider partnership, essential for long-term management success.
However, challenges persist in ensuring patient adherence, necessitating multifaceted strategies. Simplified medication regimens, reminder systems, and patient-friendly resources can enhance understanding and compliance. Utilizing glaucoma devices and digital tools, such as mobile apps for medication reminders or educational videos, caters to diverse learning preferences and lifestyles. Equally vital is the role of healthcare providers in cultivating open dialogues, addressing concerns, and tailoring treatment plans to individual needs. By fostering a collaborative approach, where patients are active participants in their care, the bridge between patient adherence and effective glaucoma management can be fortified, preserving precious vision and enhancing the overall quality of life.
Novel Glaucoma Therapeutic Targets: Expanding the Armamentarium
While existing medications effectively lower intraocular pressure (IOP), the primary risk factor for glaucoma progression, alternative therapeutic targets are needed to address non-IOP-related mechanisms. The emerging glaucoma treatment market comprises novel classes such as prostaglandin analogs, Rho-associated kinase inhibitors, Endothelin antagonists, Beta-adrenergic receptor antagonists, long-acting antiglaucoma agents, and others.
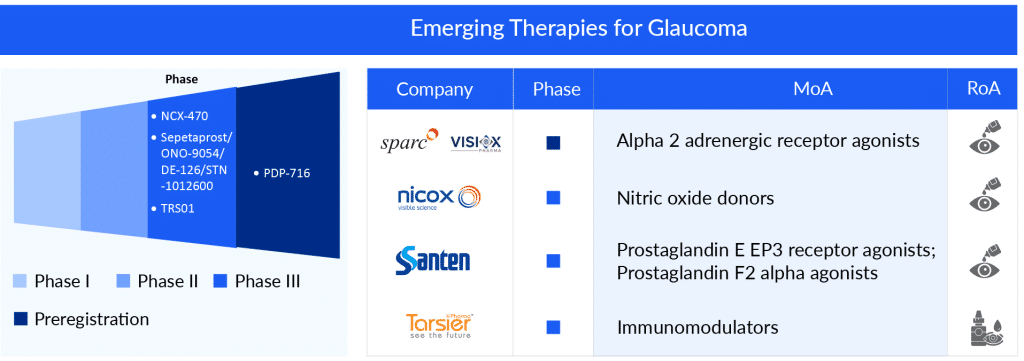
According to DelveInsight’s analysis, the current developmental pipeline for glaucoma is robust; several companies have initiated clinical trials investigating new glaucoma treatment options or studying how to use existing treatment options better.
Within this dynamic arena, several promising emerging glaucoma therapies for the effective treatment of glaucoma, such as Sepetaprost (STN1012600/DE-126) (Santen Pharmaceutical), NCX 470 (Nicox Ophthalmics), Citicoline eye drops 2% (Omikron Italia S.r.l./OPIS Spain), PDP-716 (Sun Pharma Advanced Research Company Limited (SPARC)/Visiox Pharma), and other potential glaucoma treatments.
NCX 470 represents an innovative bimatoprost eye drop that releases nitric oxide, functioning as a prostaglandin analog. Nicox Ophthalmics is the company behind its development, currently advancing it through Phase III clinical trials. The focus is on its potential for treating open-angle glaucoma or ocular hypertension within the United States. NCX 470 is engineered to deliver bimatoprost and nitric oxide upon eye application. In their recent corporate presentation, Nicox mentioned their pursuit of commercial collaborations for NCX 470 in the US and Japan.
PDP-716 is an innovative daily formulation of brimonidine created with SPARC’s TearAct technology for managing glaucoma. This glaucoma needs to be taken three times a day. Brimonidine, a widely utilized treatment for glaucoma and ocular hypertension, is the active ingredient in this drug. SPARC has partnered with Visiox Pharma to develop and market PDP-716 worldwide exclusively. Presently, the drug is undergoing Phase III clinical trials for glaucoma treatment.
STN-1012600 is a prostaglandin eye drop medication designed for once-daily use, featuring an innovative dual mode of action that stimulates both FP and EP3 receptors (both of which are prostaglandin receptors). Research suggests that these receptors play a role in reducing intraocular pressure. Therefore, STN-1012600 is anticipated to offer fresh therapeutic avenues for addressing glaucoma. Santen collaborated with Ulster University in the UK to discover, analyze, and create new and distinctive treatments for glaucoma, focusing on a facet of the immune system to restore the retina and optic nerve. This glaucoma medication is currently in Phase III of clinical trials.
In a nutshell, it is estimated that the glaucoma treatment market will experience significant changes during the forecast period of 2024–2034, owing to the launch of these new therapies that are in clinical development for the treatment of glaucoma.
Collaborative Care Models: Fostering Multidisciplinary Approaches for Glaucoma Treatment
Collaborative care models represent a pivotal shift in the approach to treating glaucoma, emphasizing the power of multidisciplinary teamwork. By bringing together ophthalmologists, optometrists, nurses, and other healthcare professionals, these models create a comprehensive framework that addresses the diverse needs of patients. In such a setup, each member contributes unique expertise, from diagnosis to treatment and ongoing management. Ophthalmologists offer specialized knowledge on surgical interventions, optometrists provide essential insights into vision correction and monitoring, while nurses ensure seamless coordination and patient education. This synergy not only enhances the quality of care but also fosters a holistic understanding of glaucoma, allowing for tailored treatments that consider both medical and lifestyle factors.
The beauty of collaborative care models lies in their ability to create a seamless continuum of care for glaucoma patients. Through regular communication and shared decision-making, healthcare professionals can ensure that patients receive timely interventions and support at every stage of their journey. This approach extends beyond the clinical setting, with an emphasis on empowering patients through education and self-management strategies. By integrating the latest research findings and technologies, these models pave the way for innovation in glaucoma treatment, promising better outcomes and improved quality of life for individuals living with this chronic condition. Ultimately, the collaborative spirit at the core of these models not only transforms the treatment landscape but also strengthens the bonds between patients and their dedicated healthcare teams.
Conclusion
Despite advancements in glaucoma treatments aimed at reducing intraocular pressure, a primary risk factor for glaucoma progression, there remains a pressing issue of unmet needs in its management. One key aspect lies in the necessity for more personalized treatment approaches, considering the diverse nature of glaucoma subtypes and patient responses. Additionally, the development of novel glaucoma therapies targeting alternative pathways beyond pressure reduction holds promise in addressing the multifaceted nature of this disease. As researchers and clinicians delve deeper into understanding glaucoma’s complexities, the quest to fulfill these unmet needs stands at the forefront of enhancing patient outcomes and preserving vision.
The launch of glaucoma emerging therapies, such as NCX 470 (Nicox Ophthalmics), PDP-716 (Sun Pharma Advanced Research Company Limited (SPARC)/ Visiox Pharma), and others are expected to impact the market positively. The total glaucoma market size in the 7MM was around USD 4 billion in 2022. This is estimated to increase by 2034 at a significant CAGR.
Furthermore, the challenge extends to improving early detection and monitoring methods, which are crucial for timely intervention. Glaucoma often remains asymptomatic until advanced stages, highlighting the critical requirement for more sensitive diagnostic tools. Advancements in imaging technologies, such as optical coherence tomography, offer valuable insights into structural changes in the optic nerve head and retinal nerve fiber layer. However, there is still a demand for innovations that enable earlier detection of glaucomatous damage, facilitating proactive treatment strategies. By addressing these unmet needs, the hope is to not only enhance the quality of life for those affected by glaucoma but also to transform the landscape of its management towards more personalized, effective, and timely care.

Downloads
Article in PDF
Recent Articles
- Analyzing the Most Promising Drugs That Will Lose Patent in the US & EU in 2022
- Alcon Gains CE Mark for Clareon Vivity IOL in Europe; MicroPort MedBot’s Toumai SP Robot Wins NMP...
- Inspira and Terumo Signed Strategic Agreement; Cook Medical’s New Bipolar Electrodes Portfolio; V...
- What can be the scope of Medical Marijuana?
- One of the leading causes of blindness, and a sight-threatening disease, Uveitis, now has novel t...