Parenteral Nutrition: A High-Growth Lifeline in Clinical Nutrition
Dec 24, 2025
Table of Contents
In the intricate landscape of healthcare, maintaining optimal nutritional status is fundamental to recovery, chronic disease management, and overall patient well-being. For millions globally who cannot ingest, digest, or absorb nutrients via the conventional gastrointestinal route, an alternative lifeline is required. This critical intervention is Parenteral Nutrition. More than just a medical procedure, PN is a meticulously crafted therapy that delivers essential sustenance directly into the bloodstream, bypassing the digestive system entirely.
The market surrounding parenteral nutrition has evolved from simple intravenous solutions to sophisticated, multi-chamber bags, driven by advancements in lipid emulsion technology, specialized amino acid formulations, and innovative delivery systems. As the prevalence of chronic diseases, gastrointestinal disorders, and severe malnutrition continues to rise worldwide, particularly in vulnerable populations like neonates and the elderly, the demand for effective PN solutions is accelerating, cementing its status as a vital, high-growth segment of the healthcare industry.
Downloads
Click Here To Get the Article in PDF
Recent Articles
- InnoCare’s Trial In China; Sanofi/GSK COVID-19 Vaccine; Apellis’s Empaveli for PNH; LianBio...
- AstraZeneca’s Voydeya FDA Approval; Akebia’s Vafseo FDA Approval; Bristol Myers Squibb’s Phase II...
- Clover’s SCB-1019 RSV Revaccination Study Clears U.S. IND; FDA Approves AMVUTTRA for ATTR-CM CV R...
- QuantuMDx & Menarini’s Agreement; TruClear System Launched by Medtronic in India; FDA 510(k)...
- Astellas & AviadoBio’s Exclusive Deal for AVB-101; GSK’s Depemokimab Shows Positive Res...
What is Parenteral Nutrition?
Parenteral Nutrition, often abbreviated as parenteral nutrition, is a medical process of supplying all or part of a person’s nutritional needs intravenously (IV). The term “parenteral” means outside the digestive tract. When a patient’s gut is unable to function, needs rest (as in some surgeries or inflammatory conditions), or cannot absorb sufficient nutrients, PN serves as the primary means of providing calories, protein, fats, vitamins, and minerals.
This therapeutic approach ensures that a patient receives the macro- and micronutrients necessary for metabolic function, tissue repair, immune defense, and energy balance. It is a highly specialized therapy that requires a multidisciplinary team, including physicians, pharmacists, dietitians, and nurses, to formulate, dispense, and monitor the individualized regimen to prevent complications and ensure efficacy.
The key differentiator of parenteral nutrition from standard IV fluids (such as saline or dextrose solutions) is its comprehensive nutrient profile. Parenteral nutrition solutions are concentrated, hypertonic mixtures designed to meet total daily energy expenditure and nutritional requirements, thereby preventing or correcting malnutrition and improving clinical outcomes. Its deployment is a testament to the sophistication of modern clinical nutrition, allowing patients with profound digestive failure to survive and thrive.
Classification of Parenteral Nutrition
Parenteral Nutrition regimens are classified primarily by route of administration, solution concentration, and nutrient packaging strategy. The distinctions are vital, as they dictate the type of venous access required and the duration for which the therapy can be safely maintained.
Total Parenteral Nutrition (TPN)
Total Parenteral Nutrition (TPN) is the most comprehensive form of PN. The term “Total” signifies that the solution provides 100% of the patient’s caloric and nutritional requirements, thus necessitating a highly concentrated formulation. Due to its high osmolarity (concentration), TPN must be infused into a large, high-flow central vein, such as the superior vena cava, via a Central Venous Catheter (CVC) or a Peripherally Inserted Central Catheter (PICC) line.
This central venous route is mandatory because high glucose and amino acid concentrations would rapidly damage the smaller, more fragile walls of peripheral veins, leading to phlebitis and thrombosis. TPN is typically employed for patients requiring long-term nutritional support or those with severe gut failure, to ensure maximum nutrient delivery efficiency and minimize the volume of fluid needed.
Peripheral Parenteral Nutrition (PPN)
Peripheral Parenteral Nutrition (PPN), also sometimes referred to by the route-specific classification, is a less concentrated PN formula designed for infusion into a peripheral vein, typically in the arm. Because peripheral veins cannot tolerate highly hypertonic solutions, PPN is volume-limited and must have a lower osmolarity, meaning the concentrations of dextrose and amino acids are significantly lower than in TPN.
Consequently, PPN can only provide partial nutritional support. It is rarely sufficient to meet an adult patient’s full caloric needs. It is primarily used for short-term nutritional support (less than 2 weeks) or as a bridge to enteral feeding when the patient still has some gut function. The main advantage of PPN is the avoidance of central venous line placement, reducing the risk of catheter-related bloodstream infections and insertion complications associated with CVCs.
Total Nutrient Admixture (TNA)
Total Nutrient Admixture (TNA), often colloquially called a “three-in-one” solution, refers to the packaging strategy of the PN formula. In a TNA, all three macronutrients, dextrose, amino acids, and lipid emulsion, are combined into a single bag or container. This is highly preferred in modern clinical practice because it simplifies the administration process, requiring only one infusion pump and one line into the patient, reducing the risk of contamination and medication errors.
TNA contrasts with “two-in-one” systems, where the lipid emulsion is infused separately from the dextrose and amino acid mixture. While ease of use is a significant benefit, TNAs require careful preparation and filtration because the combined lipids make the solution opaque, which can obscure precipitate visibility, necessitating strict quality control measures to ensure patient safety.
Components of a Parenteral Nutrition Regimen
A standard Parenteral Nutrition regimen is a complex, hypertonic solution custom-designed to mirror the balance of a healthy diet, delivering a precise mix of all essential macro- and micronutrients. The formulation must be tailored to the patient’s specific needs, including age, weight, basal metabolic rate, disease state, and organ function.
Macronutrients (Energy Sources and Building Blocks)
Carbohydrates (Dextrose): This is the primary non-protein energy source, typically provided as a highly concentrated dextrose (glucose) solution (e.g., 50% or 70%). It provides calories necessary for cellular function and helps spare protein from being broken down for energy.
Amino Acids: These are the essential building blocks for protein synthesis. They are provided as crystalline amino acid solutions, including both essential and non-essential amino acids. They are critical for tissue repair, immune function, hormone production, and enzyme synthesis. Specialized formulas exist for patients with severe liver or kidney dysfunction.
Lipid Emulsions (Fats): These provide concentrated energy (high calories per unit volume) and supply essential fatty acids (linoleic and alpha-linolenic acids), which the body cannot synthesize. Modern lipid emulsions have evolved from pure soybean oil to complex multi-oil formulations (e.g., olive oil, fish oil, and medium-chain triglycerides) to improve patient tolerance, reduce inflammation, and enhance immune response.
Micronutrients and Electrolytes
Electrolytes: Crucial for maintaining fluid balance, nerve conduction, and muscle function. These include sodium, potassium, chloride, magnesium, calcium, and phosphate. Levels are adjusted daily based on serum blood tests.
Trace Elements: Required in minute quantities but essential for enzyme activity and metabolic health. Standard supplements include zinc, copper, selenium, manganese, and chromium.
Vitamins: A comprehensive multivitamin mix is added, including water-soluble vitamins (B-complex, C) and fat-soluble vitamins (A, D, E, K). Vitamin stability in the PN bag is a significant consideration during compounding.
The combination of these components into a single, stable, and sterile solution is a highly technical process, typically overseen by specialized PN compounding pharmacists to ensure that compatibility, pH, and osmolarity are within safe and therapeutic limits.
Primary Indications for Parenteral Nutrition
The decision to initiate Parenteral Nutrition is made when the gastrointestinal tract is non-functional or when enteral feeding is inadequate or contraindicated. The main clinical goal is to prevent or reverse the debilitating effects of malnutrition. Key indications include:
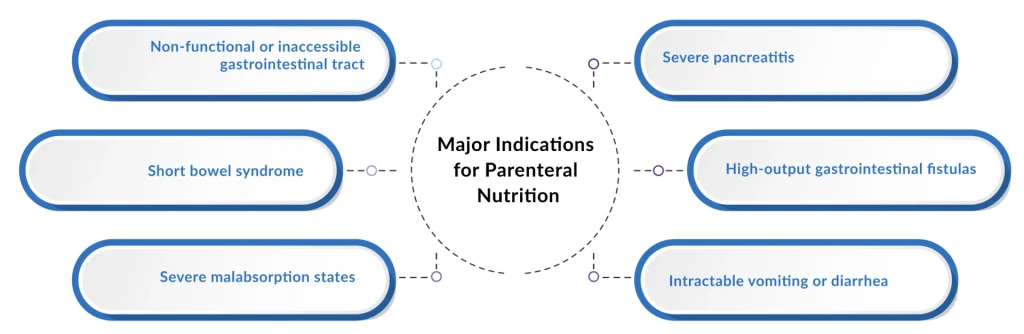
Severe Short Bowel Syndrome (SBS): Often resulting from extensive surgical resection due to Crohn’s disease, trauma, or vascular events, leaving insufficient small intestine length for nutrient absorption. Patients often rely on parenteral nutrition permanently.
Prolonged Ileus or Bowel Obstruction: When mechanical or functional blockages prevent the passage of food, parenteral nutrition allows the bowel to rest and recover while maintaining nutritional status.
Severe Malabsorption Syndromes: Conditions like severe radiation enteritis, refractory Celiac disease, or high-output intestinal fistulas (abnormal connections between the bowel and another organ/skin), where even elemental enteral diets fail to deliver sufficient nutrients.
Critical Illness and Hypermetabolic States: While enteral feeding is preferred, parenteral nutrition is indicated for critically ill patients (e.g., severe burns, major trauma) who are unable to tolerate enteral feeding for an extended period, typically exceeding 7–10 days.
Oncology: Cancer patients undergoing aggressive chemotherapy or radiation therapy, particularly those with upper gastrointestinal involvement, may require parenteral nutrition due to severe nausea, vomiting, or stomatitis that precludes oral intake.
Pediatric and Neonatal Indications: Parenteral nutrition is vital for very low birth weight (VLBW) premature infants with immature guts and for children with congenital gastrointestinal abnormalities (e.g., gastroschisis, intestinal atresia). The timely administration of PN in this group is crucial for growth and neurodevelopmental outcomes.
Benefits and Risks of Parenteral Nutrition
Parenteral Nutrition is a life-saving therapy, but its complexity means it is associated with significant potential parenteral nutrition benefits and inherent risks, all of which require meticulous management.
Primary Benefits
Life Sustaining: It is the only option for survival for patients with total intestinal failure (e.g., Short Bowel Syndrome).
Nutritional Restoration: It prevents and corrects severe malnutrition, improving patient strength, promoting wound healing, and enhancing immune function.
Bowel Rest: It allows a diseased or recently operated bowel to rest, thereby decreasing intestinal output and promoting mucosal healing in conditions such as high-output fistulas or severe inflammatory disease.
Improved Outcomes: In specific patient populations (e.g., malnourished surgical candidates), pre-operative parenteral nutrition can improve clinical outcomes and reduce complications.
Significant Risks and Complications
Catheter-Related Complications: Since parenteral nutrition requires central access, the risks include insertion complications (e.g., pneumothorax), catheter occlusion, and most significantly, Catheter-Related Bloodstream Infections (CRBSIs). Infections can be life-threatening and require catheter removal and aggressive antibiotic therapy.
Metabolic Complications: These are frequent and include hyperglycemia (high blood sugar), hypoglycemia (low blood sugar, often upon abrupt cessation), and Refeeding Syndrome, a dangerous shift in electrolytes (especially phosphate) when refeeding severely malnourished patients. Long-term use can lead to essential fatty acid deficiency and metabolic bone disease.
Liver Disease (PN-Associated Liver Disease or PNALD): A severe, long-term complication, especially in neonates and patients with underlying gut inflammation. This can range from steatosis to cirrhosis and failure. Modern lipid emulsions, particularly those containing fish oil, are used to mitigate this risk.
Gallbladder Sludge/Stones: Lack of enteral stimulation leads to biliary stasis, increasing the risk of cholelithiasis.
Careful formulation, daily laboratory monitoring, and strict aseptic technique during catheter care are non-negotiable standards for managing these risks.
Advances Shaping the Future of Parenteral Nutrition
The future of parenteral nutrition is characterized by a push toward safer, more personalized, and physiologically optimized formulations, mainly driven by advances in lipid technology and compounding automation.
One of the most impactful breakthroughs has been the development and broad adoption of Next-Generation Lipid Emulsions. Moving beyond traditional soybean oil-only products, newer structured lipids incorporating olive oil, fish oil, and medium-chain triglycerides (MCTs) have demonstrated superior outcomes. Fish oil-containing emulsions, for example, possess anti-inflammatory properties and have shown efficacy in reducing the incidence and severity of PNALD, especially in pediatric populations.
Another key area is the focus on Specialized and Personalized Parenteral Nutrition Compounding. Automation technology, including robotic compounding systems, is enhancing precision, safety, and scalability. These systems minimize human error in measuring and mixing the numerous components, ensuring sterility and accuracy of the final admixture. Furthermore, research is continually refining amino acid solutions, trace element compositions, and vitamin stability to maximize therapeutic benefit while minimizing adverse effects. This shift ensures that PN is not a one-size-fits-all therapy but a highly dynamic, individualized nutritional program.
The Role of Home Parenteral Nutrition
Home Parenteral Nutrition (HPN) represents a transformative advancement, transitioning parenteral nutrition therapy from the inpatient acute care setting to the patient’s home environment. HPN is the gold standard for managing chronic, irreversible intestinal failure, allowing patients to achieve maximum quality of life, mobility, and independence.
The patient and their caregivers are trained extensively by specialized HPN teams in aseptic techniques, catheter care, infusion pump operation, and troubleshooting. By infusing the parenteral nutrition solution overnight (typically 10-14 hours), patients are free to work, travel, and engage in social activities during the day, substantially improving psychological well-being and reducing the staggering cost of prolonged hospitalization.
The success of HPN relies heavily on robust infrastructure: reliable home care nursing support, specialized compounding pharmacies capable of delivering daily or weekly parenteral nutrition admixtures, and dedicated patient advocacy groups. As the geriatric population grows and chronic conditions necessitating lifelong PN increase, the need for scalable, safe, and cost-effective HPN programs will only continue to rise, making it a critical focus area for market growth and healthcare policy.
Future Outlook of Parenteral Nutrition
The parenteral nutrition market is poised for robust expansion, reflecting the global rise in chronic diseases and the critical need for advanced nutritional interventions. The parenteral nutrition market was valued at USD 6 billion in 2024 and is likely to register a CAGR of 6.04% from 2025 to 2032, reaching USD 8.6 billion by 2032. The parenteral nutrition market is experiencing substantial growth, primarily driven by the rising prevalence of malnutrition among children.
The primary market driver is the escalating prevalence of malnutrition among vulnerable populations, particularly children and preterm infants, alongside the increasing incidence of cancers, inflammatory bowel disease, and other chronic metabolic conditions. Key players driving innovation include industry leaders such as B. Braun SE, Fresenius Kabi, and Baxter, as well as specialized firms such as Otsuka Pharmaceutical India Pvt. Ltd, Pfizer Inc, Grifols, S.A., JW Pharmaceutical, Aculife Healthcare, Kelun, American Regent, Inc, EuroLife Healthcare Pvt. Ltd, SGD Pharma, icumedical, Generic Specialties, Vifor Pharma Management Ltd, Amanta Healthcare, Anhui Medipharm Co, Ltd, and others.
The competitive landscape is characterized by continuous R&D focus on safer lipid emulsions, pre-measured single-dose amino acid solutions, and multi-chamber bag technology to enhance convenience and safety. The future of parenteral nutrition is one of continued technological sophistication and market globalization, driven by the fundamental imperative to sustain life and foster recovery where the gut cannot.

Downloads
Article in PDF
Recent Articles
- The Evolution of Vascular Access Devices in Modern Medicine
- FDA Approves STELARA; Novartis announces AMG 334; AbbVie’s HCV Regimen; PaizaBio Gains CFDA...
- AstraZeneca’s Voydeya FDA Approval; Akebia’s Vafseo FDA Approval; Bristol Myers Squibb’s Phase II...
- Biogen terminates ALS Pact with Karyopharm; AbbVie’s Immunological Drug Skyrizi; NICE Backs Astel...
- InnoCare’s Trial In China; Sanofi/GSK COVID-19 Vaccine; Apellis’s Empaveli for PNH; LianBio...




