Insights into some of the Biosimilar Drugs that are approved and launched in 2021
Dec 15, 2021
Table of Contents
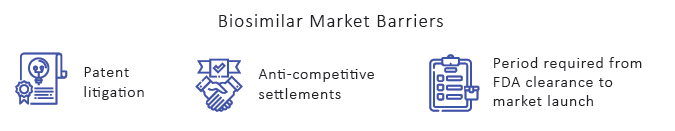
Since the first biosimilar drug was approved in 2006, the EU has led the way in biosimilar regulation. Over the last decade, the EU has authorized the most biosimilars globally, gathering significant expertise with their usage and safety. Over ten years of clinical experience has shown that biosimilars licensed by the EMA may be used as safely and effectively as other biological medicines in all of their approved indications. On the contrary, the biosimilars market in the United States has previously been described as sluggish. Patent litigation and thickets, anti-competitive settlements, and the period required from FDA clearance to market launch are barriers to biosimilar market entrance. But BPCIA, which was included in the Affordable Care Act of 2010, established a biosimilars pathway in the United States. In 2015, the US FDA authorized Zarxio, the first US biosimilar drug, whose reference biologic is Neupogen (filgrastim). As of now, the FDA has approved biosimilars corresponding to ten reference products.
Currently, biosimilars account for only 2.3% of the US biological market at the moment. Moreover, Europe accounts for 90% of worldwide biosimilars sales, even though the United States accounts for 60% of total biological sales.
Downloads
Click Here To Get the Article in PDF
Effect of COVID-19 on the US Biosimilar Market
The COVID-19 pandemic has continued to have an impact on the biopharmaceutical industry. Biosimilars are no exception, and the effect on their acceptance and uptake was multidimensional.
COVID-19 produced a massive imbalance in supply and demand, which manufacturers found challenging to predict. Manufacturing and supply chain activities in supply centers such as China, India, and the United States were interrupted as a result of worldwide lockdowns. On the demand side, confused factors made forecasting challenging. On the one hand, patients postponed seeking therapy, particularly for less convenient administration techniques such as infusions, which resulted in a decrease in patient volume and total demand. Stockpiling and desire for subcutaneous or oral formulations, on the other hand, generated a surge in demand for some medicines despite the decreased patient volume. The FDA announced the first occurrence of a medication shortage caused by a coronavirus in February 2020. Although all manufacturers attempted to reduce the danger of supply shortages, biosimilar companies that rely on facilities in Europe and Asia were more vulnerable.
Moreover, the biosimilar activity slowed in 2020 due to COVID-19 in the United States, with the lowest number of yearly biosimilar drugs approvals since 2016 and fewer product launches than in 2019—along with a decline in district court litigation and post-grant proceedings. Although the number of approvals declined in 2020, the number of development programs participating in the FDA’s Biosimilar Development Program each year has increased.
Furthermore, as a result of the global COVID-19 pandemic, the FDA has taken a number of steps, including postponing inspections. The FDA has also produced a regular stream of advice materials to assist businesses in navigating the additional obstacles posed by the pandemic. For example, in June 2020, the FDA published “Good Manufacturing Practice Considerations for Responding to COVID-19 Infection in Employees in Drug and Biological Product Manufacturing,” a guidance document that provides recommendations to drug and biological product manufacturers on manufacturing controls to prevent contamination, SARS-CoV-2 risk assessment as it relates to drug safety or quality, and manufacturing operations continuity. In August 2020, FDA issued guidance titled “Manufacturing, Supply Chain, and Drug and Biological Product Inspections During COVID-19 Public Health Emergency Questions and Answers” to clarify how FDA handles site inspections and provide insight into those inspections deemed “mission critical.” The FDA issued “Resuming Normal Drug and Biologics Manufacturing Operations During the COVID-19 Public Health Emergency” in September 2020, detailing “how to evaluate and prioritise remediation of [current good manufacturing practise (CGMP)] activities that were necessarily delayed, reduced, or otherwise modified” during the COVID-19 pandemic “in order to maintain production and the drug supply.” The FDA released recommendations in December 2020 titled “Conduct of Clinical Studies of Medical Products During the COVID-19 Public Health Emergency,” which addresses safety and compliance with good clinical practice (GCP) in clinical trials done during COVID-19.

Biosimilar Approval and Launches in 2021
2021 brings a number of biosimilar drugs approvals and product launches. We have witnessed the approval of the first insulin biosimilar. Several new entrants are also expected to enter the Humira market in the coming years. Let’s look at some of the top biosimilar approvals and launches that happened in 2021.
Riabni
The FDA has authorized Amgen’s Riabni (rituximab-arrx), a biosimilar to Rituxan (rituximab), for the treatment of adults with Non-Lymphoma Hodgkin’s (NHL), Chronic Lymphocytic Leukemia (CLL), Granulomatosis with Polyangiitis (GPA) (Wegener’s Granulomatosis), and Microscopic Polyangiitis (MPA) in December 2020. From January 2021, Riabni is available in the United States biosimilar market. Riabni will be accessible in the United States at a Wholesale Acquisition Cost (WAC) of USD 716.80 per 100 mg and USD 3,584.00 per 500 mg single-dose vial, which is 23.7% less than the WAC for the original Rituxan and the same as the WAC for Ruxience (another rituximab biosimilar). Riabni’s clearance represents Amgen’s fifth biosimilar approval by the FDA.
Cyltezo
In October, the US FDA authorized the first interchangeable biosimilar drug to treat certain inflammatory disorders. Cyltezo (adalimumab-adbm) manufactured by Boehringer Ingelheim, was authorized in August 2017 and is both biosimilar to and interchangeable with its reference medicine Humira (adalimumab) for Cyltezo’s approved uses. Cyltezo is the agency’s second interchangeable biosimilar product and the first interchangeable monoclonal antibody. Once on the market, licensed biosimilar and interchangeable biosimilar medications can help to improve access to therapies for a variety of important health diseases. Cyltezo has FDA approval for rheumatoid arthritis, juvenile idiopathic arthritis, psoriatic arthritis, ankylosing spondylitis, Crohn’s disease, ulcerative colitis, and plaque psoriasis.
Cyltezo is also approved for moderately to highly active polyarticular juvenile idiopathic arthritis in children aged two and up, as well as Crohn’s disease in children aged six and up. Cyltezo is injected subcutaneously (under the skin) under the supervision of a physician in a single-dose, pre-filled glass syringe (40 mg/0.8 mL, 20 mg/0.4 mL).
Hanbeitai
The National Medical Products Administration on December 2021 approved Hanbeitai; a bevacizumab biosimilar developed and manufactured by Henlius. It is approved for the treatment of metastatic colorectal cancer (mCRC) and unresectable, locally advanced, recurring, or metastatic non-squamous non-small cell lung cancer (non-squamous non-small cell lung cancer) (nsNSCLC). Hanbeitai is the fourth monoclonal antibody (mAb) biosimilar authorized by the firm in China, following rituximab biosimilar Hanlikang, trastuzumab biosimilar Hanquyou (ZercepacR in the EU), and adalimumab biosimilar Handayuan. The pipeline has been expanded to include further indications, such as hematological malignancies, solid tumors, and auto-immune disorders.
SEMGLEE and Insulin Glargine Injection
Viatris Inc and Biocon Biologics have launched interchangeable biosimilars SEMGLEE (insulin glargine-yfgn) injection, a branded product, and Insulin Glargine (insulin glargine-yfgn) injection, an unbranded product, in the US biosimilar market in November to assist manage high blood sugar in adult and pediatric patients with type 1 diabetes and adults with type 2 diabetes. Both biosimilar medications are available in a vial and prefilled pen formats and are interchangeable with the reference brand, Lantus (insulin glargine), enabling substitution at the pharmacy counter. Semglee (insulin glargine-yfgn) is the first interchangeable biosimilar product approved for the treatment of diabetes in the United States. The currently available non-interchangeable SEMGLEE (insulin glargine) is expected to be phased out by the end of 2021.
Byooviz
Byooviz is the first biosimilar to Lucentis (ranibizumab) to be approved in the United States and Europe. It got the FDA approval in September whereas got the EMA approval in August. Byooviz was developed by Samsung Bioepis and will be commercialized by Biogen in the European Union, the United States, and certain other markets.
Byooviz has been approved to treat neovascular (wet) age-related macular degeneration, diabetic macular edema, proliferative diabetic retinopathy, macular edema secondary to retinal vein occlusion, and choroidal neovascularization.
The EU authorization comes after the EMA’s Committee for Medicinal Products for Human Use recommended approval for the indications mentioned above on June 24, 2021. (CHMP). CHMP conducts preliminary evaluations of marketing authorization applications and changes to existing authorizations, including marketing authorization modifications, suspensions, or withdrawals. (Explore more about the Biosimilar Market Landscape in Europe)
Onbevzi
Onbevzi, a biosimilar to Avastin (bevacizumab) developed by Samsung Bioepis, has been launched in Korea by Boryung Pharmaceutical in September. Boryung acquired the exclusive sales rights to Onbevzi in Korea from Samsung in May. Onbevzi is the first biosimilar in Korea for Avastin, Roche’s anticancer drug. Metastatic colorectal cancer, metastatic breast cancer, non-small cell lung cancer, advanced or metastatic renal cell carcinoma, glioblastoma, epithelial ovarian cancer, fallopian tube or primary peritoneal cancer, and cervical cancer are among the indications for which Onbevzi has approved.
Furthermore, Boryung Pharmaceutical, which has the largest market share for anticancer drugs among local pharmaceutical companies, intends to target the 120 billion won annual bevacizumab market in Korea, based on Onbevzi’s product excellence and differentiated anticancer drug sales and marketing competitiveness.
Yuflama
Celltrion’s adalimumab biosimilar, Yuflyma, had received European Commission (EC) approval in February. Adalimumab is used to treat rheumatoid, juvenile idiopathic, and psoriatic arthritis, as well as ankylosing spondylitis (AS), Crohn’s disease, psoriasis, and ulcerative colitis.
The European Commission’s (EC) approval comes after the European Medicines Agency’s (EMA) Committee for Medicinal Products for Human Use (CHMP) positive recommendation on December 11, 2020. The EC approval is based on analytical, preclinical, and clinical studies that show Yuflyma is safe, effective, and comparable to the reference product in terms of pharmacokinetics, pharmacodynamics, and immunogenicity up to 24 weeks and one year after treatment.
Yuflyma is the tenth adalimumab biosimilar to be approved in Europe. The European Commission’s clearance is valid in all EU member states, as well as Iceland, Liechtenstein, and Norway, which are part of the European Economic Area (EEA). Celltrion also announced on February 17, 2021, the launch of Remsima SC, a subcutaneous version of its infliximab biosimilar. Remsima SC was first introduced in Europe (Germany and the United Kingdom) in February 2020.
Kixelle
Kixelle, a biosimilar Insulin Aspart (Novo Nordisk) co-developed by Viatris and Biocon, received marketing authorization approval from the European Commission in February, following a positive recommendation from the European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP). Kixelle is the second insulin aspart biosimilar to be approved in the EU. Kixelle, a fast-acting insulin analog indicated for the treatment of type 2 diabetes in adults, adolescents, and children aged 1 year and older, has been approved as a 100 unit/ml injection solution in vial and pre-filled pen forms.
The EC’s centralized marketing authorization is valid in all EU Member States as well as Iceland, Liechtenstein, and Norway, which are European Economic Area (EEA) members.
What’s Next?
Biosimilars have gained a significant share of the market in the vast majority of therapeutic areas where they have been introduced. Additional competition can result in substantial savings for the healthcare system, which can then be used to fund newer, more innovative treatments. The development of biosimilar pathways in the United States, Europe, and other parts of the world provides healthcare systems with the opportunity to realize cost savings associated with a more competitive biologic drug marketplace rather than the higher pricing associated with a monopolist manufacturer. Multiple rivals on the market are the greatest approach to obtain these savings since it brings prices closer to the marginal cost of manufacturing these drugs, making them more accessible. Several advancements in this space are expected over the next few years, including the expansion of biosimilars into pharmacy benefit reimbursement, biosimilars in more classes, and the approval of interchangeable biosimilars in the United States. Several new players are also expected to enter the Humira market in the upcoming years.
FAQs
Byooviz is the first biosimilar to Lucentis (ranibizumab) to be approved in the United States and Europe. It got the FDA approval in September whereas got the EMA approval in August. Byooviz was developed by Samsung Bioepis and will be commercialized by Biogen in the European Union, the United States, and certain other markets.
The US FDA authorized the first interchangeable biosimilar drug to treat certain inflammatory disorders in October. Cyltezo (adalimumab-adbm) manufactured by Boehringer Ingelheim, was authorized in August 2017 and is both biosimilar to and interchangeable with its reference medicine Humira (adalimumab) for Cyltezo’s approved uses.
Patent litigation and thickets, anti-competitive settlements, and the period required from FDA clearance to market launch are barriers to biosimilar market entrance. But BPCIA, which was included in the Affordable Care Act of 2010, established a biosimilars pathway in the United States.
Semglee (insulin glargine-yfgn) is the first interchangeable biosimilar product approved for the treatment of diabetes in the United States. The currently available non-interchangeable SEMGLEE (insulin glargine) is expected to be phased out by the end of 2021.
Key players such as Amgen, Boehringer Ingelheim, Henlius, Viatris Inc, Biocon, Samsung Bioepis, Biogen, Boryung Pharmaceuticals, Celltrion, and others are currently working in the biosimilar market.
Downloads
Article in PDF
Recent Articles
- Biosimilars: A benchmark in Pharmaceutical Business
- EMA to relocate to Amsterdam; Roche’s prospects; Amgen’s Humira Biosimilar delayed; Purdue’s opio...
- Changing Landscape of EBV-associated Diseases Treatment: Is T-cell Immunotherapy the Answer?
- Wet AMD: A chronic eye condition with promising therapies
- Could Hidradenitis Suppurativa Be Another Psoriasis?