AI Hospitals of the Future–Where Robotics, Predictive Analytics, and Compassion Converge
Nov 05, 2025
Table of Contents
The global healthcare landscape is undergoing one of the most transformative revolutions in modern history. At the heart of this evolution lies Artificial Intelligence (AI), a force that is not just augmenting medical workflows but reshaping how hospitals function, how care is delivered, and how humanity interacts with medicine itself.
In the hospitals of the future, algorithms will predict disease before symptoms appear, robots will assist surgeons with microscopic precision, and virtual companions will comfort patients recovering in smart wards. Yet amid all this technology, compassion will remain the defining constant, the human essence amplified, not replaced, by machines.
These AI-powered hospitals represent a convergence of robotics, predictive analytics, digital twins, and precision medicine, turning healthcare into a seamlessly integrated ecosystem of intelligence, empathy, and innovation.
Downloads
Click Here To Get the Article in PDF
Recent Articles
- Non-Surgical Body Contouring: What’s Fueling Its Growth in Aesthetic Medicine?
- Medical Radiation Detection Devices: Essential Tools in Healthcare and Diagnostics
- How is Artificial Intelligence (AI) Playing a Constructive Role in Mental Health Management?
- Cancer Diagnostic Market: Evaluating the Major Growth Factors and the Key Developments in the Domain
- 22 Healthcare Trends & Innovations to Watch in 2022 and Beyond
The Rise of the AI Hospital: From Reactive Care to Predictive Healing
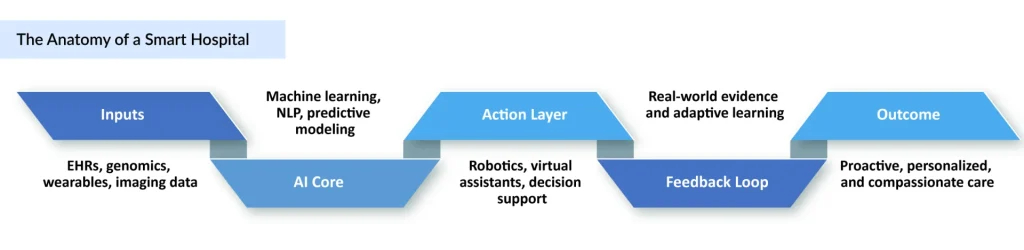
Traditionally, hospitals have been centers of treatment, places where patients come after illness strikes. The AI hospital of the future will invert that model entirely, becoming a hub of predictive and preventive care. Through advanced data analytics, machine learning, and real-time patient monitoring, these intelligent health systems will identify health risks before they escalate, optimizing care delivery and resource allocation.
AI-driven predictive models can analyze vast datasets, including electronic health records (EHRs), genomic data, wearable device data, and even social determinants of health, to forecast disease trajectories. For example, a patient’s continuous blood pressure, heart rate, and oxygen data could alert clinicians to early signs of cardiac distress long before an emergency occurs. Similarly, AI algorithms could anticipate hospital readmission risks, guiding personalized discharge plans and follow-ups.
In essence, the AI hospital will move from reactive medicine to proactive well-being, using intelligence to anticipate rather than just respond. The future of healthcare will not just treat disease, it will prevent it.
Robotics and Automation: Redefining Precision and Efficiency
Inside AI hospitals, robots will no longer be confined to operating theaters; they will be integral to nearly every department. Surgical robots, already a reality through systems like da Vinci and CorPath GRX, will evolve into autonomous assistants guided by AI vision and tactile sensors, capable of performing microsurgeries at sub-millimeter precision.
Beyond surgery, logistical and service robots will manage pharmacy dispensing, laboratory transport, and even patient assistance. These robotic systems, synchronized through AI-driven hospital command centers, will streamline workflows, reduce human error, and allow healthcare professionals to focus on the human aspects of care.
In emergency and intensive care units, robotic arms paired with AI analytics will assist clinicians with critical tasks such as drug administration, wound care, and airway management. Meanwhile, social robots equipped with natural language processing (NLP) and emotion recognition capabilities will offer companionship to elderly or isolated patients, bridging the gap between clinical efficiency and emotional support.
By 2035, it is anticipated that AI and robotics could automate up to 30% of hospital operations, not by replacing healthcare workers but by relieving them of repetitive, data-intensive, or physically demanding tasks, creating an environment where human compassion can flourish alongside machine precision.
Predictive Analytics: The Brain of the Smart Hospital
If robotics is the muscle of the AI hospital, predictive analytics is its brain. Powered by deep learning and real-world data, predictive systems continuously analyze patient information to anticipate medical events, resource demands, and treatment outcomes.
Consider intensive care units (ICUs), where real-time AI models continuously process thousands of physiological data points to predict sepsis onset hours before visible symptoms. In oncology wards, predictive algorithms analyze genomic data, treatment history, and tumor biology to personalize chemotherapy protocols, maximizing therapeutic efficacy while minimizing toxicity.
Hospitals like Mayo Clinic, Mount Sinai, and Apollo Hospitals are already experimenting with AI-driven command centers, digital “nervous systems” that use predictive dashboards to optimize everything from bed occupancy and operating room schedules to ambulance routing and supply chain management.
In the future, AI hospitals will function as self-learning organisms, constantly refining their processes through feedback loops and real-world evidence. Every patient interaction, prescription, and lab result will feed into models that evolve with time, ensuring healthcare delivery becomes increasingly adaptive and intelligent.
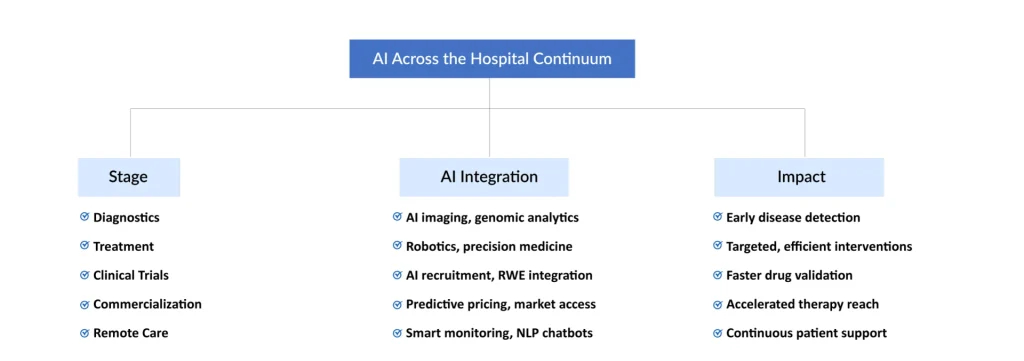
AI in Diagnostics: The Foundation of Early Detection
No futuristic hospital can function without AI-driven diagnostics, the core that enables early detection and intervention. In recent years, Artificial Intelligence (AI) in Cancer Diagnostics has demonstrated how machine learning models can identify subtle imaging patterns undetectable to the human eye. AI systems trained on millions of radiological and pathological scans are achieving diagnostic accuracies rivaling top specialists, especially in detecting cancers of the lung, breast, and skin.
These intelligent systems not only enhance accuracy but also reduce diagnostic turnaround time, a critical factor in time-sensitive diseases. AI-powered imaging tools, combined with cloud-based integration, will enable instant collaboration among global specialists, allowing remote diagnosis and second opinions within minutes.
Beyond oncology, AI in life sciences is bridging genomics, proteomics, and clinical data, empowering hospitals to tailor treatments at a molecular level. Algorithms are now capable of predicting disease predispositions based on genomic variants, leading to the rise of AI in precision medicine, where therapy decisions are guided by individualized biological profiles rather than population averages.
As diagnostic intelligence advances, hospitals will evolve into hubs of integrated detection and prevention, where diseases are identified before they become clinically visible, a transformation that could redefine healthcare.
AI in Clinical Trials: Hospitals as Research Powerhouses
Tomorrow’s AI hospitals will not just treat patients, they will actively participate in drug discovery and clinical research. The integration of AI in clinical trials will make hospitals key nodes in decentralized research networks, enabling faster patient recruitment, adaptive trial design, and real-time safety monitoring.
Traditionally, clinical trials are slowed by recruitment inefficiencies and data fragmentation. AI algorithms can overcome these barriers by matching eligible patients to trials using EHR data, genomic profiles, and prior treatment history. Real-world data from AI hospitals will further enrich trial outcomes, enabling continuous learning between the bedside and the bench.
Hospitals will partner with pharmaceutical companies to use AI in drug discovery and AI in drug commercialization, creating a full-circle ecosystem, from molecule design to market deployment, driven by data intelligence. In this ecosystem, the hospital becomes both a care center and a digital laboratory, where every patient contributes to advancing global therapeutic knowledge.
Remote Patient Monitoring and the Hospital Beyond Walls
One of the defining features of AI hospitals will be their ability to extend care beyond physical infrastructure. Through Artificial Intelligence (AI) in Remote Patient Monitoring, continuous data streams from wearable sensors, smart implants, and home devices will feed into hospital analytics systems, enabling real-time patient tracking even outside the facility.
AI will detect anomalies, such as arrhythmias, glucose spikes, or respiratory distress, and trigger alerts to physicians or caregivers instantly. For chronic disease management, these systems will personalize care plans based on behavioral and physiological data, reducing hospital readmissions and improving quality of life.
This concept of the “virtual hospital” is already emerging through digital-first health systems like Mercy Virtual in the U.S. and Apollo’s Health@Home initiative in India. Over time, the AI hospital will become a hybrid ecosystem, where digital and physical care merge seamlessly, empowering continuous, data-driven wellness across geographies.
Humanizing the AI Hospital: Compassion in the Age of Algorithms
One of the greatest misconceptions about AI in healthcare is that it might diminish human empathy. In reality, AI hospitals will humanize medicine by freeing clinicians from administrative overload, allowing them to focus on what machines cannot replicate, which is compassion, communication, and connection.
With AI handling repetitive documentation, billing, and diagnostic triage, physicians will have more time to engage with patients, explain conditions, and provide emotional support. Emotional AI systems, equipped with NLP and sentiment analysis, will further enable empathetic virtual assistants to understand patient tone and mood, offering both clinical and emotional assistance.
In mental health wards, AI-powered chatbots are already providing early intervention and cognitive behavioral support. These tools don’t replace therapists but serve as companions that bridge gaps, ensuring care remains constant, even when human interaction isn’t immediately available.
Thus, the AI hospital is not a sterile machine fortress; it’s a compassionate digital sanctuary, where intelligence and empathy coexist to deliver truly patient-centered care.
Data, Ethics, and Trust: Building Responsible AI Hospitals
The success of AI hospitals depends not only on technology but also on trust and ethical governance. With vast amounts of sensitive data flowing through interconnected systems, ensuring privacy, fairness, and transparency becomes paramount.
Hospitals will need to adopt robust ethical AI frameworks aligned with global standards such as GDPR, HIPAA, and the FDA’s AI/ML regulatory guidelines. Continuous algorithm auditing, bias mitigation, and explainability will form the foundation of responsible intelligence.
Bias in training data, if unchecked, can result in disparities in diagnosis or access. Hence, future hospitals will invest in diverse data collection, inclusive model design, and human oversight to maintain equity in AI-driven decisions.
Furthermore, data sharing among hospitals, pharmaceutical companies, and research organizations will require secure interoperability frameworks supported by blockchain and federated learning, enabling insights to be shared without compromising patient privacy.
In the AI hospital of tomorrow, transparency will be the currency of trust, ensuring that intelligent systems serve every patient fairly, safely, and ethically.
The Global Outlook: Toward a Learning Healthcare System
Globally, nations are investing heavily in AI-driven healthcare infrastructure.
- The United States leads with smart hospital pilots integrating AI into operational command centers and diagnostics.
- Europe is leveraging its European Health Data Space initiative to build interconnected AI health networks.
- Asia-Pacific, led by China, Japan, and India, is rapidly scaling AI-driven precision hospitals as part of national digital health missions.
By 2032, analysts expect the AI in healthcare market to grow significantly, with hospitals accounting for a large share of that growth. AI hospitals will deliver higher efficiency, lower costs, and better outcomes, enabling sustainable healthcare systems even amid aging populations and rising chronic disease burdens.
But beyond economics lies a more profound transformation: the creation of a learning healthcare system, one that continuously evolves, learns from every patient encounter, and applies that knowledge to improve care for all. AI hospitals will form the neural network of this system, connecting care, research, and innovation into a single living organism.
Looking Ahead: The Symbiosis of Humanity and Machine
The future hospital will not be a place; it will be a dynamic ecosystem.
One where AI systems guide precision therapies, robots perform intricate procedures, predictive analytics prevent crises, and virtual care transcends physical walls.
Yet, at its core, it will remain profoundly human.
The promise of AI in healthcare isn’t to replace empathy with efficiency, but to enhance both. The AI hospital of the future is where Artificial Intelligence meets human intelligence, where data and compassion converge, and where medicine finally fulfills its most fundamental mission, to heal, prevent, and care.
As we step into this era, the boundaries between technology and humanity will blur, not because machines become more human, but because humans, empowered by machines, will become more capable, compassionate, and connected than ever before.
In the end, the hospitals of the future will not just save lives, they will redefine what it means to live well.
Downloads
Article in PDF
Recent Articles
- The Revolution of Healthcare: Smart Medical Devices Transforming the Future
- From Paper to Pixels: The Advantages and Challenges of Electronic Health Record
- The Automated Eye: How AI-Driven Diagnostics are Reshaping the Future of Medical Imaging
- Viz.ai’s AI Algorithm for Abdominal Aortic Aneurysm; BrainTale Unveils the New Version of I...
- FDA Breakthrough Device Designation to Pi-Cardia’s ShortCut; AbSolutions Med’s REBUILD Bioabsorba...