Medtronic Diabetes Announced FDA Clearance for MiniMed Go™ Smart MDI System Featuring Instinct Sensor Made by Abbott
On January 12, 2026, Medtronic, a global leader in healthcare technology, announced that it had received U.S. Food and Drug Administration (FDA) 510(k) clearance for its MiniMed Go™ app. The MiniMed Go™ Smart Multiple Daily Injection (MDI) system was designed to seamlessly integrate the InPen™ smart insulin pen with the Instinct sensor from Abbott, all connected through the MiniMed Go™ app. Together, this integrated system provided real-time, personalized insights and actionable guidance, including missed dose alerts to help reduce glucose spikes, a dose calculator to simplify insulin decision-making, guidance when a dose was missed or miscalculated, and CareLink™ software reporting to support collaboration between patients and healthcare providers.
The MiniMed Go™ system was cleared for individuals aged 7 years and older with insulin-requiring type 1 and type 2 diabetes, as well as for children aged 2 to 6 years when used under adult caregiver supervision. At the time of the announcement, compatibility of the Simplera™ sensor with MiniMed Go™ remained under FDA review.
Globally, more than 15 million people with diabetes relied on multiple daily injections, and for many, managing insulin dosing around meals was mentally demanding and stressful. This daily burden, which involved estimating carbohydrate intake and calculating appropriate insulin doses, often contributed to distress in people with diabetes. Missed insulin boluses have a significant impact on diabetes management, with research indicating that skipping just two doses per week can increase HbA1c by up to 0.4%, thereby increasing the risk of both short- and long-term complications.
Real-world evidence from users of Medtronic’s previous-generation Smart MDI system demonstrated meaningful improvements in glycemic control when users consistently responded to actionable alerts. The data showed that Time in Range (TIR) improved from 55.7% to 67.2% when users addressed more than 75% of missed-dose alerts within 1 hour, and further to 71.5% when users responded to high-glucose alerts with a bolus within 1 hour. These findings highlighted the value of timely, actionable insights in improving glycemic outcomes. Building on this evidence, the MiniMed Go™ Smart MDI System was introduced to deliver enhanced, real-time, personalized guidance to optimize diabetes management for users.
“For too long, people using injections have carried the weight of diabetes management without access to the algorithms that make automated insulin delivery systems so powerful,” said Que Dallara, EVP and president of Medtronic Diabetes and CEO-designate of MiniMed. “MiniMed Go™ is designed to change that bringing the smarts of an AID system to individuals who prefer an insulin pen. The system helps take the guesswork out of MDI therapy, delivering simplicity and confidence in every dose. We’re pleased to expand our full-stack insulin delivery solutions, making it seamless for our customers to find a therapy that works for them — no matter where they are in their journey.”
As per DelveInsight’s “Diabetes Care Devices Market Report,” the global diabetes care devices market size was valued at USD 34.28 billion in 2024 and is expected to reach USD 66.82 billion by 2032, at a CAGR of 8.70 % during the forecast period. The diabetes care devices market is driven by a combination of clinical, demographic, technological, and healthcare-system factors. A major driver is the rising global prevalence of diabetes, particularly type 2 diabetes, fueled by aging populations, sedentary lifestyles, obesity, and unhealthy dietary habits. The growing emphasis on early diagnosis and continuous disease management has increased demand for blood glucose monitors, continuous glucose monitoring (CGM) systems, insulin pumps, and smart insulin pens. Technological advancements, such as real-time CGMs, closed-loop or artificial pancreas systems, mobile app integration, and data-driven decision support, are improving accuracy, convenience, and patient adherence, thereby accelerating device adoption. Additionally, increasing awareness among patients and healthcare providers, supportive government initiatives and reimbursement policies, and the shift toward home-based and self-care management are boosting device usage. The expansion of digital health and telemedicine, especially for remote diabetes monitoring, along with rising healthcare expenditure in both developed and emerging economies, further supports market growth by improving access to advanced diabetes care technologies.
Neurolief Received FDA PMA Approval for First At-Home Brain Neuromodulation Therapy for Adults Whose Depression was not Adequately Improved by Antidepressants
On January 12, 2026, Neurolief Inc., a medical device company specializing in neuromodulation therapies for neuropsychiatric conditions, announced that it had received U.S. Food and Drug Administration (FDA) approval for Proliv™Rx. Proliv™Rx became the first prescription, physician-directed, at-home brain neuromodulation therapy approved as an adjunctive treatment for adults with Major Depressive Disorder (MDD) who had not achieved adequate improvement after at least one prior antidepressant medication.
The approval was granted through the Class III Premarket Approval (PMA) pathway and was supported by clinical evidence from the MOOD Study, a randomized, controlled, multicenter clinical trial that evaluated the safety and effectiveness of Proliv™Rx in patients with MDD who had an inadequate response to antidepressant therapy.
This regulatory milestone provided clinicians and health systems with a scalable next-step treatment option when medications failed, allowing clinically validated brain neuromodulation to be administered at home under physician supervision. By enabling home-based therapy, Proliv™Rx helped address access limitations and reduced the infrastructure and operational burdens typically associated with clinic-based neuromodulation interventions.
“Until now, patients struggling with difficult-to-treat depression did not have a non-pharmacological therapy option that could be administered at home”, said Linda Carpenter, MD, Principal Investigator of the MOOD clinical trial, Professor of Psychiatry at Brown University and Director of the Neuromodulation Program at Butler Hospital. “Even though there is a tremendous need for new treatment approaches when antidepressant medications aren’t working, access to interventional psychiatry services like Transcranial Magnetic Stimulation (TMS) remains limited. Now we can offer our patients Proliv™Rx therapy with continued medical supervision and the convenience of home use. Not only does Proliv™Rx introduce a novel mechanism for noninvasive neuromodulation through its actions on the occipital and trigeminal neural pathways, but it also establishes a new treatment paradigm by making evidence-based neuromodulation widely accessible, beyond the walls of the specialty clinic”.
As per DelveInsight’s “Neuromodulation Devices Market Report,” the global neuromodulation devices market is expected to increase from USD 7,862.04 million in 2024 to USD 16,111.10 million by 2032, reflecting strong and sustained growth. The global neuromodulation devices market is projected to grow at a CAGR of 9.44% from 2025 to 2032. The market for neuromodulation devices is growing rapidly, fueled by the rising global prevalence of chronic diseases like pain, epilepsy, and depression. This growth is also driven by significant technological advancements that have made devices smaller, smarter, and more effective. Favorable regulatory policies and better reimbursement coverage are also making these treatments more accessible. Overall, the growing demand for effective, long-term therapeutic options for neurological and chronic conditions is driving a strong, sustained market.
Haemonetics Acquired Vivasure Medical Limited
On January 09, 2026, Haemonetics Corporation, a global medical technology company focused on improving patient outcomes, announced that it had acquired Vivasure Medical Limited, a Galway, Ireland–based company specializing in next-generation percutaneous vessel closure technologies. Vivasure’s PerQseal® Elite system uses a proprietary bioabsorbable patch to seal large-bore arteriotomies and venotomies (up to 26 F) from within the vessel, offering a sutureless, fully absorbable solution for structural heart and endovascular procedures.
In 2025, Vivasure submitted a Premarket Approval (PMA) application to the U.S. Food and Drug Administration (FDA) for the PerQseal Elite arterial closure system and had also received CE Mark approval in Europe for both arterial and venous indications. Clinical evidence from the prospective, single-arm, multicenter ELITE arterial study demonstrated the system’s ease of use without the need for pre-close techniques, with zero major complications at 30-day follow-up and an immediate median time to hemostasis.
Under the terms of the transaction, Haemonetics agreed to make an upfront cash payment of €100 million, or approximately €52 million net after accounting for the value of certain prior investments and loans provided to Vivasure, along with customary closing adjustments. The deal also included the potential for up to €85 million in additional contingent consideration, tied to future sales growth and the achievement of specified milestones, and subject to adjustments related to earlier investments and loan amounts. Haemonetics financed the acquisition using available cash on hand.
“Acquiring Vivasure expands Haemonetics’ complete range of closure devices with new and clinically differentiated technology to bolster our presence in the large-bore closure market and our impact in fast-growing structural heart and endovascular procedures,” said Ken Crowley, Vice President & General Manager, Interventional Technologies at Haemonetics. “With strong clinical performance and safety data, PerQseal Elite positions us for increased leadership in advanced closure, as we leverage our commercial scale and operational synergies to deliver increased value to physicians and hospitals.”
As per DelveInsight’s “Vascular Closure Devices Market Report,” the global vascular closure devices market is expected to increase from USD 1,548.87 million in 2024 to USD 2,398.52 million by 2032, reflecting strong and sustained growth growing at a CAGR of 5.70% during the forecast period from 2025 to 2032. The market for vascular closure devices is primarily driven by the increasing prevalence of cardiovascular diseases and associated risk factors, the growing adoption of minimally invasive procedures, technological advancements in devices, and an increase in product development activities among key market players.
Boston Scientific Announced Agreement to Acquire Valencia Technologies Corporation
On January 12, 2026, Boston Scientific Corporation announced that it had entered into a definitive agreement to acquire Valencia Technologies Corporation, a privately held medical technology company focused on developing and commercializing innovative treatments for bladder dysfunction. Valencia’s flagship product, the eCoin® System, was an implantable tibial nerve stimulation (ITNS) device designed to treat urge urinary incontinence (UUI), a common symptom of overactive bladder (OAB).
In the United States, nearly 30 million adults aged 40 years and older were affected by bothersome OAB symptoms, a condition known to significantly impact quality of life, mental health, sleep, productivity, and social activities. Despite this high prevalence, studies had shown that the overall treatment rate for OAB beyond behavioral and lifestyle modifications was only about 19%, highlighting a substantial unmet clinical need.
The eCoin system, which received U.S. Food and Drug Administration approval in 2022, was a coin-sized implant placed under the skin near the ankle through a minimally invasive procedure. It was intended for patients who had either responded successfully to a trial of percutaneous tibial nerve stimulation (PTNS) or who were unable to tolerate or had an inadequate response to more conservative UUI therapies. Once implanted, the device automatically delivers intermittent stimulation to the tibial nerve, helping regulate communication between the brain and the bladder. In the pivotal eCoin clinical trial, 68% of patients achieved at least a 50% reduction in UUI episodes.
Boston Scientific expected to complete the acquisition in the first half of 2026, subject to customary closing conditions. The transaction was expected to have an immaterial impact on adjusted earnings per share in 2026, but would be more dilutive on a GAAP basis due to acquisition-related charges and amortization expenses. The specific financial terms of the agreement were not disclosed.
According to DelveInsight’s “Urology Devices Market Report”, the global urology devices market is expected to increase from USD 34,898.97 million in 2024 to USD 63,320.19 million by 2032, reflecting strong and sustained growth, growing at a CAGR of 7.77% during the forecast period from 2025 to 2032. The global urology devices market is growing due to the rising prevalence of kidney stones, urinary incontinence, BPH, and prostate and bladder cancers, particularly among the aging population. Advancements in minimally invasive and robotic-assisted procedures, along with improved diagnostics, are boosting adoption. Additionally, increasing healthcare spending, expanding infrastructure in emerging economies, and rising lifestyle-related risk factors such as obesity and diabetes are further driving market demand.
Butterfly Medical Announced Completion of Pivotal Trial for Minimally Invasive Treatment of Benign Prostatic Hyperplasia
On January 08, 2026, Butterfly Medical, a developer of a proprietary non-surgical solution for benign prostatic hyperplasia (BPH), announced the successful completion of the final 12-month follow-up for all patients enrolled in its international pivotal clinical study. The landmark study assessed the safety and effectiveness of the Butterfly Prostatic Retraction Device, which was positioned as a first-line interventional therapy (FIT) for the treatment of BPH.
The Butterfly Prostatic Retraction Device was designed to conform to the prostate’s natural anatomy and restore urinary flow without cutting, burning, or removing tissue. The prospective, double-blind, randomized controlled trial (RCT) enrolled 244 patients to evaluate the device, a minimally invasive, reversible implant that mechanically retracts the lateral lobes of the prostate to improve urinary flow in patients with BPH symptoms.
BPH was recognized as one of the most prevalent conditions among aging men, affecting approximately 50% of men aged 51–60 and up to 90% of men over 80 years of age. Despite its high prevalence, a large portion of patients remained underserved. Existing drug therapies typically required long-term use and were associated with side effects such as dizziness and sexual dysfunction, while conventional surgical treatments often involved invasive tissue removal, leading to notable side effects and extended recovery periods.
“This trial marks a critical step in validating the Butterfly Prostatic Retraction Device as a safe and effective solution that avoids the limitations of early-generation BPH treatments,” said Patrick MacCarthy, CEO of Butterfly Medical. “Combined with our multi-year follow-up data presented last year, this study shows great promise for the Butterfly device as a durable, long-term solution for men suffering from the symptoms of BPH. Thanks to the support of our many clinical collaborators and of course all 244 patients, we are well positioned to address a significant unmet need in the global urology market.”
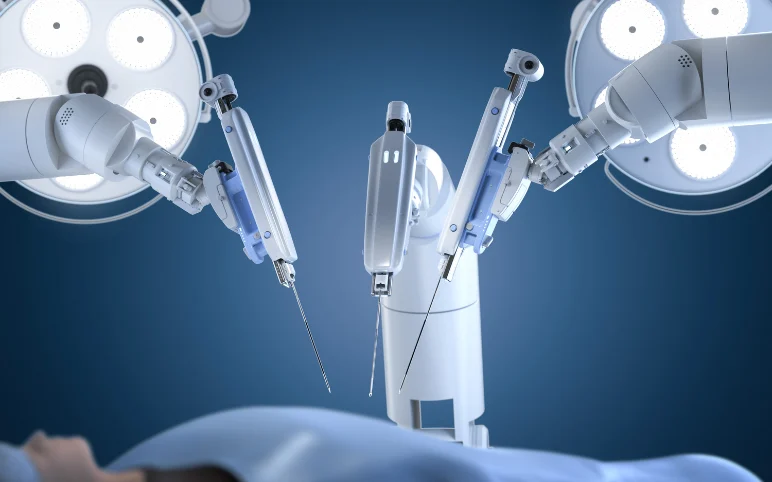
According to DelveInsight’s ”Minimally Invasive Surgical Devices Market Report,” the global minimally invasive surgical devices market is expected to increase from USD 30,798.01 million in 2024 to USD 53,259.85 million by 2032, reflecting strong and sustained growth, is growing at a CAGR of 7.13% during the forecast period from 2025 to 2032. The market for minimally invasive surgical devices is primarily driven by the rising prevalence of chronic diseases such as cancer and cardiovascular disorders, technological advancements in surgical devices, and an increase in product development activities among key market players globally.
TYBR Health Announced the First U.S. Clinical Use of the B3 GEL™ System
On January 05, 2026, TYBR Health, a regenerative medicine and medical device company focused on improving post-surgical soft-tissue healing, announced the first U.S. clinical use of the B3 GEL™ System. The initial procedure was performed by Dr. Hanna Tammam, a fellowship-trained hand, elbow, and shoulder surgeon based in Lubbock, Texas, and marked an important milestone in translating advanced biomaterial science into routine clinical practice.
The B3 GEL™ System was designed to improve postoperative tendon mobility through an intuitive, precise proprietary delivery mechanism, enabling surgeons to achieve functional outcomes while integrating seamlessly into existing surgical workflows.
B3 GEL™ was a collagen-based tissue protector derived from extracellular matrix (ECM). Unlike traditional physical barrier products that could be challenging to deploy in confined anatomical spaces, the B3 GEL™ System was flowable, conformed to tissue surfaces, and maintained biomechanical separation during the critical healing period, after which it was naturally resorbed. Recently published research on ECM-based hydrogels suggested these materials may positively interact with the early healing environment, supporting the body’s natural repair processes. TYBR Health continued to evaluate the clinical performance of the B3 GEL™ System through post-market surveillance and real-world clinical use.
“In a complex second-stage flexor tendon reconstruction where balancing tissue protection with early rehabilitation is critical I applied B3 GEL™ directly over the repair,” said Dr. Hanna Tammam. “The gel set within minutes, maintained excellent visualization, and allowed smooth tendon gliding without restricting motion. I subsequently used it in two additional flexor tendon repair cases, and across these early cases I observed consistently favorable early range of motion, minimal stiffness, and no complications—findings that are very encouraging in this patient population.”
“The first cases in the United States with the B3 GEL™ System represent a pivotal milestone for TYBR Health and for patients undergoing musculoskeletal surgeries”, said Chris Wright, Chief Commercial Officer of TYBR Health. “These initial procedures mark the transition from regulatory clearance to real-world clinical application, allowing surgeons to directly address post-surgical tissue tethering a complication that too often limits patient mobility and extends recovery times. By protecting healing tissues during the critical early phase, B3 GEL™ helps bridge the gap between surgical repair and functional success, enabling patients to regain movement faster and more completely. We’re excited to see these early outcomes that support our mission of improving quality of life for millions affected by tendon, ligament, and muscle procedures.”
TYBR Health continued to expand the clinical adoption of the B3 GEL™ System in collaboration with surgeons and conducted post-market surveillance studies to collect real-world evidence on the system’s performance and patient outcomes across a variety of surgical settings.
According to DelveInsight’s “Surgical Sealant and Adhesives Market Report”, the global surgical sealant and adhesives market was valued at USD 2.18 billion in 2023, growing at a CAGR of 7.58% during the forecast period from 2024 to 2030 to reach USD 3.39 billion by 2030. The surgical sealant and adhesives market is slated to grow owing to the rising prevalence of chronic health conditions, including cardiovascular, kidney, and neurological disorders. The rise in road accidents requiring urgent surgeries is another factor in the growth of the surgical sealant and adhesives market. The continuous rise in cosmetic surgeries and the growing focus on improving the safety, affordability, and usability of surgical sealants and adhesives are further expected to result in appreciable revenue growth in the Surgical Sealant and Adhesives Market during the forecast period 2024 to 2030.