Brain-Computer Interface (BCI) Applications Driving Healthcare Innovation
Oct 06, 2025
Table of Contents
Brain-Computer Interfaces (BCIs) are emerging as a groundbreaking technology in the healthcare sector, offering innovative solutions for patients with neurological disorders, spinal cord injuries, and other debilitating conditions. A BCI is a direct communication pathway between the brain and external devices, enabling users to control computers, prosthetics, or other assistive technologies using neural signals. In healthcare, BCIs are revolutionizing neurorehabilitation, assistive technologies, and patient monitoring, making previously impossible interventions possible.
One of the most compelling applications of BCIs is in neurorehabilitation for stroke patients and individuals with spinal cord injuries. By translating neural activity into commands, BCIs help patients regain motor functions, control robotic exoskeletons, or operate prosthetic limbs, dramatically improving quality of life. BCIs also play a critical role in restoring communication for patients with locked-in syndrome or severe paralysis, enabling them to interact with computers, speech-generating devices, or smartphones using brain signals alone.
Downloads
Click Here To Get the Article in PDF
Recent Articles
- Innovative Solutions, Lifesaving Possibilities: Evaluating the Artificial Organs Market Dynamics
- Norlase’s ECHO™ Green Pattern Laser; HAPPE Spine’sINTEGRATE-C™ Interbody Fusion Sys...
- Roche Receives FDA Approval for Itovebi; FDA Approves Bausch + Lomb’s Envista® Envy™; Microbot Me...
- Noninvasix’s LIVOx™ Central Venous Oxygenation Monitor; LivaNova’s aura6000 System; Oxford...
- Edwards’s Pascal Precision System; Abbott’s New Spinal Cord Stimulation Device; Imagin to A...
In addition, BCIs are increasingly being integrated with mental health and neurofeedback therapies, allowing clinicians to monitor brain activity in real-time and provide personalized treatments for conditions like depression, anxiety, and ADHD. The use of BCIs in early detection and monitoring of neurological disorders, including Alzheimer’s disease, Parkinson’s disease, and epilepsy, is also gaining traction, providing clinicians with actionable insights for proactive care.
Furthermore, the combination of BCIs with artificial intelligence (AI) and machine learning enhances the accuracy and responsiveness of these systems, enabling predictive analytics, adaptive control of assistive devices, and tailored therapy plans. As research and clinical trials expand, BCIs are poised to become a standard part of personalized healthcare solutions, improving patient outcomes and expanding the possibilities of medical innovation.
Overall, brain-computer interfaces are not just a futuristic concept; they are actively reshaping the healthcare landscape by enhancing patient mobility, communication, and cognitive function, making them a critical technology for the next generation of medical treatments.
Working Mechanism of Brain-Computer Interface in Healthcare
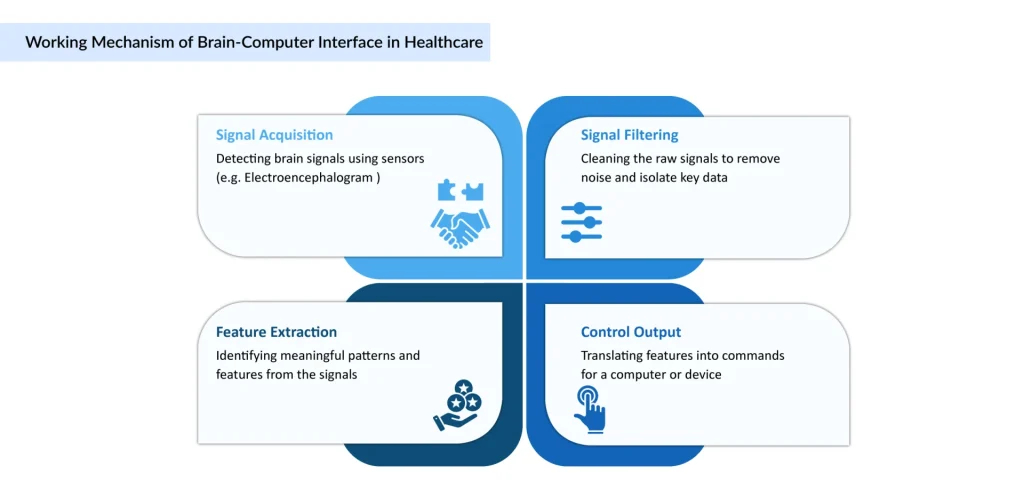
The core function of a BCI follows a sophisticated four-step process, translating neural signals into actionable commands for external devices.
Brain-Computer Interfaces function by creating a direct communication link between the brain and external devices without relying on the body’s normal pathways of nerves and muscles. In healthcare, this mechanism allows patients with neurological disorders, paralysis, or cognitive impairments to regain mobility, communication, and independence.
The process involves four main steps:
1. Brain Signal Acquisition
- BCIs detect brain activity using either invasive or non-invasive methods.
- Non-invasive techniques like EEG (Electroencephalography), fNIRS (functional Near-Infrared Spectroscopy), or MEG (Magnetoencephalography) record electrical activity from the scalp.
- Invasive techniques use implanted electrodes directly in the brain to capture more precise signals.
- In healthcare, non-invasive EEG-based BCIs are most commonly used due to their safety and lower risks.
2. Signal Processing and Feature Extraction
- The raw brain signals are extremely complex and noisy.
- Advanced algorithms filter these signals to identify specific neural patterns linked with motor intention, emotional states, or cognitive tasks.
- For example, if a stroke patient thinks about moving their arm, the BCI detects that motor intention pattern.
3. Translation Algorithms
- Machine learning and artificial intelligence convert the processed brain signals into commands that an external device can understand.
- This translation allows thoughts to be turned into actions, for example, moving a robotic prosthetic limb, operating a wheelchair, or typing on a computer screen.
4. Device Output and Feedback
- The translated commands control external devices such as:
- Prosthetics – brain-controlled robotic arms or legs.
- Communication devices – speech-generating software for paralyzed patients.
- Neurorehabilitation systems – exoskeletons or virtual reality therapies for stroke recovery.
- Patients receive feedback (visual, auditory, or haptic), which helps them adjust their thoughts and improve accuracy over time.
Types of Brain-Computer Interface in Healthcare
| Feature | Invasive Brain-Computer Interface (BCI) | Non-Invasive Brain-Computer Interface (BCI) |
|---|---|---|
| Definition | Involves surgical procedures to place high-fidelity electrode arrays directly onto or into brain tissues. Direct contact allows precise reading of neural signals from specific brain regions like the motor cortex. | Common and safer as they do not require surgery. Typically use external headset or cap with sensors that rest on the scalp to record brain activity, most commonly using electroencephalography (EEG). |
| Advantages | Unmatched signal quality and high precision control. | Safe, accessible, convenient, and easy to use. |
| Disadvantages | Requires brain surgery and carries risk of infection and scarring. | Lower signal quality and limited control precision. |
| Major Applications | Amyotrophic Lateral Sclerosis, Spinal Cord Injury, Stroke, Parkinson’s Disease, Severe Speech Impairments | Stroke Rehabilitation, Epilepsy, Sleep Disorders, Depression, Neurorehabilitation, ADHD, Autism |
5 Million+: Individuals with paralysis who could benefit from BCI technology
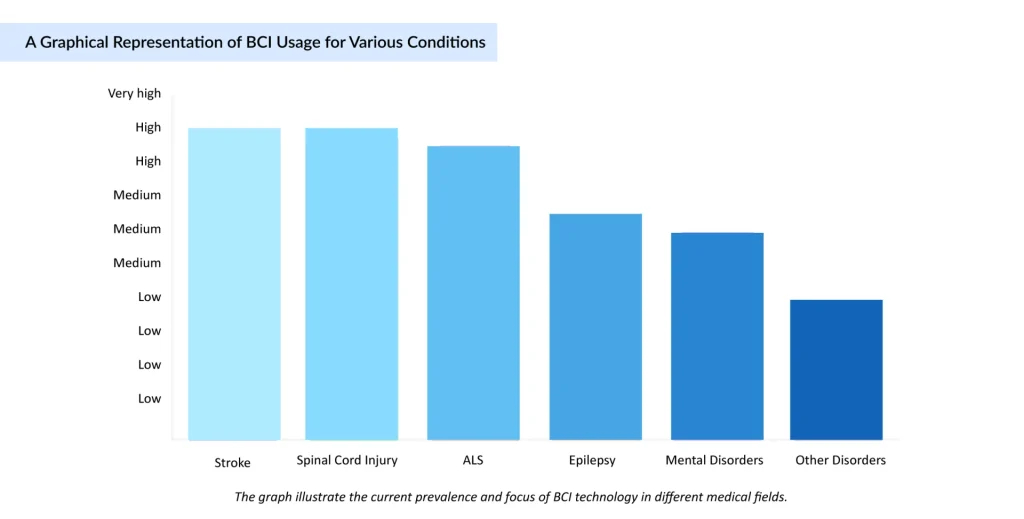
Major Applications Where the Brain-Computer Interface in Healthcare is Mostly Used
- Stroke – One of the most common applications of BCIs, it helps in neurorehabilitation, where BCIs detect motor intention and guide robotic exoskeletons or virtual therapies to restore arm and leg movements, and improve recovery of motor skills by retraining neural pathways. According to the data provided by recent studies (2024), there were approximately 93.8 million prevalent cases and 11.9 million incident cases of strokes.
| Disease / Condition | Recent Example & What was Done | Key Outcome / Significance |
| Stroke (Motor Rehabilitation) | Efficacy of brain-computer interface training with motor imagery-contingent feedback among persons with chronic stroke: a randomized controlled trial published January 2025. Participants with chronic stroke used BCI training with feedback to improve upper-limb function. | Demonstrated measurable improvement in motor function and neuroplasticity. Validates that BCI + motor imagery + feedback can help post-stroke patients regain limb control. |
- Amyotrophic Lateral Sclerosis (ALS) – ALS patients gradually lose voluntary muscle control. BCIs provide communication tools, allowing patients to type, use speech-generating devices, or control computers using only brain activity. According to the data provided by the Centers for Disease Control and Prevention (2025), in 2022, cases of ALS in the US were close to 33,000 cases, and by 2030, these cases will rise by more than 10% to over 36,000 cases.
| Disease / Condition | Recent Example & What was Done | Key Outcome / Significance |
| ALS / Speech-Impairment | Neuralink’s trial for speech impairments (speech cortex implant), clinical trials starting October 2025, aimed at converting “thoughts” into text for patients with speech impairment (stroke, ALS, etc.) | Promises to bypass traditional communication barriers; could enable patients to communicate via thought-to-text with minimal delay. |
- Spinal Cord Injury – BCIs bypass damaged spinal pathways to restore mobility and control. Patients can use brain signals to control wheelchairs, robotic limbs, or assistive devices. According to the data provided by the World Health Organization (2024), over 15 million people were living with spinal cord injury.
| Disease / Condition | Recent Example & What was Done | Key Outcome / Significance |
| Spinal Cord Injury / Paralysis | Chinese clinical trial: a man who lost all four limbs can play chess & racing games using his mind only, after an invasive BCI implant. (Shanghai, 2025) | Demonstrates potential for severely paralyzed patients to regain interactive control in digital environments; shows stable implant operation. |
- Other Disorders – According to the data provided by the World Health Organization (2024), approximately 970 million people globally were living with a mental disorder.
According to the data provided by the World Health Organization (2024), an estimated 5 million people are diagnosed with epilepsy each year.
| Disease / Condition | Recent Example & What was Done | Key Outcome / Significance |
| Mood / Mental Health / Neurodegenerative | NHS trial of brain-implant using ultrasound (Forest Neurotech) to boost mood / treat depression/epilepsy / OCD, etc.; mapping and influencing neuron clusters. | Exploring less invasive / non-electrode methods; potential new treatments for psychiatric & mood disorders. |
| Speech after Stroke | An experimental brain-computer implant enabling a stroke survivor (47 years old, speech lost 18 years) to speak again in real time by decoding imagined speech into fluent sentences. | Very strong example of restoring speech long after a stroke; might set the path for more devices for aphasia/loss of speech. |
| Epilepsy / Seizure Detection | “Personalization on a Budget: Minimally-Labeled Continual Learning for Resource-Efficient Seizure Detection”, a DL framework that adapts to patient-specific EEG signals, with few labeled data, and good performance. | Real‐time/adaptive seizure detection could reduce false alarms and make wearable or home devices more viable. |
BCIs help in seizure detection and prediction by analyzing abnormal neural activity. Provides early warning systems that can alert patients or trigger responsive neurostimulation to prevent seizures. BCIs combined with neurofeedback therapy allow patients to visualize and regulate their brain activity and are used in personalized mental health treatments by monitoring emotional and cognitive states.
How can a BCI Overcome the Challenges of People With Neurological Disorders?
Traditional therapies often fall short in fully restoring function. Brain-Computer Interfaces (BCIs) provide a revolutionary solution by directly linking brain activity to external devices, bypassing damaged neural pathways. Here’s how BCIs address these challenges:
| Challenge Faced by Patients | BCI Solution / Mechanism | Outcome / Benefit |
| Loss of motor function (stroke, spinal cord injury) | Detects motor intentions from brain signals; controls robotic exoskeletons, prosthetic limbs, or virtual rehabilitation tools | Improved limb mobility, faster recovery, enhanced independence. |
| Inability to communicate (ALS, locked-in syndrome, severe stroke) | Decodes neural signals for speech or intent; enables typing, speech generation, or communication device control | Restored communication, social interaction, and reduced emotional isolation. |
| Cognitive deficits, attention problems, depression, anxiety, PTSD | Neurofeedback and BCI-assisted cognitive therapy; monitors and regulates brain activity | Improved focus, emotional control, and cognitive rehabilitation |
| Risk of seizures or disease progression (epilepsy, Parkinson’s) | Real-time EEG monitoring; detects abnormal brain activity; predicts seizures | Timely interventions, reduced emergencies, proactive disease management |
| Dependence on caregivers for daily activities | Brain-controlled wheelchairs, smart home devices, robotic assistants; AI integration for adaptive control | Greater autonomy, improved quality of life, and reduced caregiver dependence. |
| Personalized rehabilitation and treatment | Collects real-time neural data; AI analyzes patient-specific brain patterns; tailors therapy. | More effective, patient-specific interventions, accelerated research |

Recent Development Activities of the Brain Computer Interface in Healthcare
- In August 2025, the FDA granted 510(k) clearance for Precision Neuroscience’s Layer 7-T Cortical Interface. The minimally invasive device, featuring 1,024 electrodes through a micro-slit smaller than 1 mm, provided clinicians with high-resolution brain interface capabilities, expanding possibilities in neurosurgical and research applications.
- In June 2025, A Chinese man who lost all four limbs in a high-voltage accident 13 years ago was able to play chess and racing games using only his mind after undergoing China’s first-in-human invasive BCI implant in Shanghai. Implanted in March 2025, the device operated stably with no reported infections or electrode failures, marking a key step in moving BCI technology from research to clinical use.
- In June 2025, A research team at the University of Michigan completed the first in-human recording using Paradromics Inc.’s Connexus wireless brain-computer interface (BCI). The dime-sized device, containing 421 microelectrodes thinner than a human hair, was temporarily implanted during a temporal lobectomy in a patient with epilepsy, recording brain signals to help restore functions lost due to injury or disease.
- In September 2024, Elon Musk’s brain-computer interface implant startup Neuralink received FDA breakthrough device designation for Blindsight, an implant that aims to restore vision in individuals who are blind.
- In September 2025, Siemens Healthineers partnered with Mayo Clinic to develop AI-enhanced digital twins in cardiovascular care. These models are designed to simulate patient-specific responses and predict heart complications using real-time health records and imaging.
Brain Computer Interface in Healthcare Industry: Market Overview and Dynamics
The global brain-computer interface (BCI) in healthcare market was valued at USD XX million in 2024 and is projected to reach USD XX million by 2032, growing at a CAGR of XX% from 2025 to 2032. Key factors driving this growth include the rising prevalence of neurological disorders such as stroke, ALS, spinal cord injuries, and Parkinson’s disease, increasing demand for assistive technologies, advancements in AI and neural signal processing, and the growing adoption of minimally invasive and non-invasive BCI solutions to restore motor and cognitive functions.
In 2024, North America dominated the market due to the presence of leading BCI technology developers, advanced healthcare infrastructure, supportive government research funding, and collaborations between technology companies (like Neuralink, Blackrock Neurotech, and Paradromics) with hospitals and research institutions. The U.S. is at the forefront of clinical BCI adoption, particularly in applications such as motor rehabilitation, communication devices for paralyzed patients, and neuroprosthetics.
Europe is emerging as a key market, driven by an emphasis on improving care for neurological disorders, integration of AI in clinical workflows, and stringent regulatory standards encouraging safe deployment of neural interface technologies. Countries like Germany, France, and the U.K. are investing heavily in neurotechnology research, clinical trials, and rehabilitation centers integrating BCIs for patient care and clinical research.
The Asia-Pacific region is projected to be the fastest-growing market due to increasing healthcare digitization, large populations affected by neurological disorders, government-backed innovation programs, and growing adoption of neurorehabilitation devices in countries such as China, Japan, and India. Rising awareness of assistive technologies and expansion of clinical BCI trials are creating opportunities for both invasive and non-invasive neural interface devices.
From a solution perspective, the market is segmented into:
- Invasive BCIs (implanted electrodes for high-resolution neural signal acquisition, used in spinal cord injury rehabilitation, motor function restoration, and communication aids for locked-in patients).
- Non-invasive BCIs (EEG or fNIRS-based devices for neurofeedback, stroke recovery, cognitive rehabilitation, and gaming/therapeutic applications).
- Semi-invasive BCIs (epidural or subdural electrodes for seizure monitoring, motor rehabilitation, and neuroprosthetic control).
- BCI software and platforms (signal processing, machine learning algorithms, and neural decoding software for controlling prosthetics, wheelchairs, communication devices, or brain-stimulation therapies).
Integration with AI, machine learning, robotics, and cloud-based platforms is transforming BCIs into highly adaptive systems capable of real-time brain signal decoding, predictive neurofeedback, and personalized rehabilitation. As healthcare increasingly focuses on patient-centric and precision neurology solutions, BCIs are becoming pivotal in restoring lost motor, sensory, and cognitive functions and enabling new therapeutic approaches for neurological disorders.
Brain Computer Interface in Healthcare Market Dynamics
Market Drivers
- Restoration of Motor and Cognitive Functions: BCIs enable patients with paralysis, spinal cord injuries, or neurodegenerative disorders to regain control over movement, communication, and daily activities. This capability drives adoption in neurorehabilitation and assistive technologies.
- Advancements in AI and Neural Signal Processing: Integration of AI and machine learning with BCI devices allows real-time decoding of brain signals, improving accuracy and responsiveness of prosthetics, wheelchairs, communication aids, and neurofeedback therapies.
- Rising Prevalence of Neurological Disorders: Increasing cases of stroke, Amyotrophic Lateral Sclerosis, Parkinson’s disease, epilepsy, and traumatic brain injuries have created demand for solutions that restore lost functions, boosting the clinical adoption of BCI technologies.
- Minimally Invasive and Non-Invasive Solutions: The development of wireless, implantable, and wearable BCIs reduces surgical risks and improves patient acceptance, expanding use in both clinical and home-based rehabilitation.
- Integration with Robotics and Rehabilitation Devices: Combining BCIs with robotic exoskeletons, prosthetics, and therapeutic devices enhances patient outcomes in motor recovery and enables personalized rehabilitation programs.
Market Restraints
- Data Security and Privacy Concerns: BCIs collect highly sensitive neural data. Breaches or unauthorized access to brain signal data raise ethical and regulatory concerns, creating adoption barriers.
- High Costs and Technical Complexity: Implantable and high-resolution BCI systems require sophisticated hardware, signal processing algorithms, and clinical expertise, making them expensive and difficult for smaller hospitals or clinics to implement.
- Regulatory and Ethical Challenges: Clinical approval for invasive BCIs involves rigorous testing due to safety and long-term implantation concerns. Ethical issues regarding neural data usage and patient consent may also slow adoption.
- Interoperability Challenges with Existing Clinical Systems: Integrating BCI outputs with electronic health records, rehabilitation platforms, and hospital IT systems is complex, delaying seamless clinical workflow integration.
Future of Brain Computer Interface in Healthcare
The future of Brain-Computer Interfaces (BCIs) in healthcare is poised to redefine patient care, rehabilitation, and disease management by leveraging advances in neurotechnology, artificial intelligence, and wearable devices. BCIs are expected to evolve from primarily experimental and niche applications to mainstream clinical tools for neurological disorders, such as stroke, spinal cord injury, ALS, Parkinson’s disease, epilepsy, and dementia. With improvements in signal resolution, wireless technology, and non-invasive methods, BCIs will become safer, more reliable, and accessible for a broader range of patients.
In rehabilitation, BCIs will enable personalized neurofeedback and motor training programs, accelerating recovery and enhancing neuroplasticity. For communication, thought-to-text and speech synthesis systems will allow patients with severe paralysis or speech impairments to regain independence and social interaction.
Additionally, integration with artificial intelligence and machine learning will allow BCIs to predict seizures, monitor cognitive decline, and optimize treatment strategies in real time.
Beyond neurological disorders, BCIs are expected to expand into psychiatry, pain management, sleep therapy, and cognitive enhancement, bridging the gap between mental and physical healthcare. Regulatory approvals and commercial launches over the next decade will likely drive widespread adoption, while ethical considerations, data privacy, and equitable access will shape the responsible deployment of these technologies.
Overall, BCIs hold the promise of transforming healthcare into a more proactive, personalized, and connected system, improving outcomes and quality of life for millions of patients worldwide.
Conclusion
In conclusion, Brain-Computer Interfaces (BCIs) represent a groundbreaking frontier in healthcare, offering unprecedented opportunities to restore motor function, enable communication, and enhance cognitive and emotional well-being for patients with neurological and other complex disorders. By directly linking brain activity to external devices, BCIs bypass damaged neural pathways, allowing individuals with paralysis, stroke, ALS, or severe speech impairments to regain independence and improve their quality of life.
The integration of non-invasive and invasive technologies, along with advances in artificial intelligence and neurofeedback, continues to expand the scope and precision of BCIs, making them increasingly accessible and practical for clinical applications. As research progresses and regulatory approvals grow, BCIs are set to transform rehabilitation, patient monitoring, and personalized treatment, while also opening doors for broader applications in mental health, pain management, and cognitive enhancement.
Ultimately, BCIs embody the convergence of neuroscience, engineering, and digital technology, heralding a new era of patient-centered care where the boundaries between mind and machine are seamlessly bridged.
FAQs
A Brain-Computer Interface (BCI) is a technology that enables direct communication between the brain and external devices. BCIs detect neural activity and translate it into commands, allowing users to control computers, prosthetic limbs, wheelchairs, or communication devices using thought alone.
BCIs work by recording brain signals through invasive methods (implanted electrodes) or non-invasive methods (EEG, fNIRS, MEG). These signals are processed by algorithms to decode user intentions, which are then used to control external devices or software in real time.
There are two major types:
Invasive BCIs: Implanted directly into the brain; they offer high precision for severe neurological conditions.
Non-Invasive BCIs: Use external sensors like EEG; safer and widely used for rehabilitation, monitoring, and neurofeedback.
EEG (Electroencephalography) records brainwave patterns non-invasively from the scalp. In BCIs, EEG detects motor intentions, attention, and cognitive states, which are processed to control devices, assist in rehabilitation, or provide neurofeedback.
Yes. BCIs allow patients to control prosthetic limbs, wheelchairs, communication devices, and smart home systems using thought alone, significantly reducing reliance on caregivers and enhancing quality of life.
Downloads
Article in PDF
Recent Articles
- Bioventus’s StimRouter Pain Management Device; FDA Approval for eCoin Therapy; SurGenTec Launches...
- Eosolutions Corp’s Dr. Banner Balloon Guide Catheter; US FDA Approves the Cyltezo® Pen; Orlucent’...
- Vagus Nerve Stimulators Market Outlook
- Beta Bionics Introduces iLet Bionic Pancreas with Abbott’s FreeStyle Libre 3 Integration; Merit M...
- ABANZA Secures FDA 510(k) Clearance for WasherCap™ Mini; Cerus Corporation Secures CE Mark for Ne...