The Hidden World of Vision: Exploring the Top 5 Rare Eye Diseases
Oct 16, 2023
Table of Contents
Rare diseases affect a larger population than cancer and AIDS combined, with over 7,000 distinct conditions impacting more than 300 million globally. Approximately 1 in 10 individuals are affected by a rare disease, and it often requires several years to receive an accurate diagnosis, averaging around 4.8 years. Approximately 95% of rare diseases lack an FDA-approved treatment. Numerous rare eye conditions have a genetic basis, making it challenging to discover effective treatments. While these rare eye diseases affect only a small portion of the population, their impact on those affected can be substantial. The limited information available for accurate diagnosis and subsequent treatment poses a significant hurdle for both patients and healthcare providers. Given that specific treatments for most of these conditions are unavailable, early diagnosis emerges as the most effective strategy to minimize their impact on the affected individual’s health.
Challenges in Treating Rare Eye Diseases
Treating rare eye diseases poses a myriad of challenges that significantly burden both patients and the healthcare system. One of the foremost challenges lies in the limited availability of treatment options. Unlike more common eye conditions, rare diseases often lack dedicated research and development efforts, resulting in a dearth of approved therapies. This scarcity forces patients to navigate a complex maze of potential treatments, some of which may be experimental or require substantial financial resources to access. Additionally, the rarity of these conditions can make it difficult to find specialized healthcare providers with expertise in managing and treating such diseases, further adding to the patient’s burden.
Downloads
Click Here To Get the Article in PDF
Recent Articles
- From Sight to Insight: The Rise of Smart Ophthalmological Devices in Eye Care
- FDA Approves Sarepta’s Muscular Dystrophy Drug after Months of Debate
- HUTCHMED’s NDA Submission to FDA for Fruquintinib; Cytokinetics to Discontinue ALS Drug Candidate...
- Celltrion Announces FDA Nod for New STEQEYMA Presentation to Broaden Pediatric Use; CSL’s ANDEMBR...
- DelveInsight’s Gene Therapy Reports: Launched
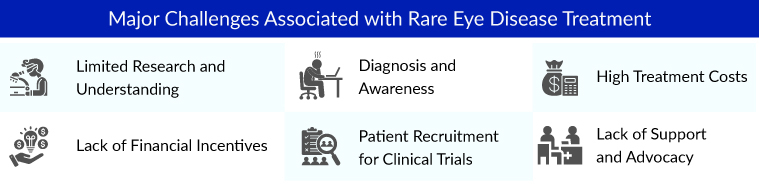
Moreover, the cost of treatment for rare eye diseases can be exorbitant. Due to the low prevalence of these conditions, there is often no incentive for pharmaceutical companies to invest in research and development, making drugs and interventions exceptionally costly. This places an immense financial strain on patients and their families, who may need to pay out-of-pocket for treatments that are not covered by insurance. The burden is further compounded by the emotional toll rare eye diseases take on patients, as they often face a lack of support and understanding from their immediate community and may struggle with feelings of isolation and uncertainty. These challenges underscore the urgent need for increased awareness, research, and support systems for individuals affected by rare eye diseases.
Top 5 Rare Eye Diseases
There are several eye diseases that can pose a burden on thousands of patients across the world. The top rare eye diseases with a genetic basis causing trouble to most people and their families include Stargardt Disease, Retinitis Pigmentosa, Leber Hereditary Optic Neuropathy (LHON), Retinoblastoma, and Limbal Stem Cell Deficiency. Let’s dive deep into the assessment of these rare eye diseases individually.
Stargardt Disease
Stargardt disease, also known as Stargardt macular dystrophy, is attributed to its discovery by the German ophthalmologist Karl Stargardt in 1901. It is alternatively referred to as juvenile macular degeneration or fundus flavimaculatus. This condition falls under the category of rare retinal disorders with an autosomal recessive inheritance pattern. The predominant causal factor for Stargardt disease is genetic mutations within the ABCA4 gene. According to the American Institute of Ophthalmology (2023), Stargardt disease accounts for about 7% of all retinal degeneration, grossly affecting 1 per 10,000 individuals.
Stargardt disease currently lacks approved treatments, and existing therapeutic options do not address its underlying cause. Researchers are exploring three primary avenues for intervention, including clinical trials involving stem cell therapy, gene replacement therapy, and pharmacological approaches. Additionally, some ophthalmologists recommend protective measures such as wearing sunglasses and hats in bright light to minimize lipofuscin accumulation. Avoiding cigarette smoking and secondhand smoke is also advisable. High-dose vitamin A supplements, beyond the recommended daily allowance, could potentially exacerbate vision loss based on animal studies, making them inadvisable without proper medical supervision.
Stargardt disease presents a significant medical challenge since there are presently no approved treatments. Consequently, there is a pressing demand for novel therapies aimed at retarding the disease’s progression and preserving visual acuity over an extended period. Promisingly, several emerging therapies in the Stargardt disease pipeline, include Kubota Pharmaceuticals (Emixustat), Alkeus Pharmaceuticals (ALK-001), Astellas Pharma (ASP7317/Avacincaptad pegol [ACP]), and others.
Emixustat (Kubota Pharmaceuticals) is an oral drug that originally targeted the dry form of age-related macular degeneration and works by slowing the buildup of toxic waste products that lead to retinal degeneration in a number of retinal conditions, including Stargardt disease. The European Medicines Agency (EMA) and FDA have granted orphan designation to Acucela’s leading drug candidate Emixustat hydrochloride (emixustat) for the treatment of Stargardt disease. It is drug completed the Phase III trial in July 2022. In October 2022, the company announced positive results from a post hoc analysis of the phase III clinical trial.
Astellas’s stem cell treatment (ASP7317) is designed to protect and regenerate photoreceptors in the retina that are damaged by eye diseases like Stargardt’s. It is currently in Phase I clinical trials and has been granted Orphan Drug Designation for Stargardt disease.
The dynamics of the Stargardt disease treatment market are anticipated to change in the coming years. As per DelveInsight analysis, the Stargardt disease treatment market is expected to grow positively at a significant CAGR by 2032 owing to the launch of these therapies and the rise in the number of healthcare spending across the world.
Retinitis Pigmentosa
Retinitis pigmentosa is a collective term for a cluster of genetic eye disorders impacting the retina, the light-sensitive region of the eye. Retinitis pigmentosa initiates the deterioration of photoreceptor cells, which are responsible for detecting light. The initial damage typically targets rod cells, and this variant of retinitis pigmentosa is often referred to as rod-cone dystrophy, manifesting with night vision problems. As per DelveInsight analysis, in 2022, the diagnosed prevalent population of retinitis pigmentosa in the 7MM was 260K. These diagnosed cases are further divided into three types: Syndromic and Systemic retinitis pigmentosa, Non-syndromic retinitis pigmentosa, and other or unknown types of retinitis pigmentosa.
Currently, standard treatment options do not exist for individuals with retinitis pigmentosa. Nevertheless, there are available treatments for an exceptionally rare variant of retinitis pigmentosa, and ongoing research is actively exploring novel therapies such as gene therapy, transplantation, and implanted electrical devices to manage certain clinical manifestations.
Luxturna stands out as the sole officially sanctioned retinitis pigmentosa treatment for an exceedingly uncommon variant of retinitis pigmentosa available in both the United States and European markets. It has the potential to put a stop to vision deterioration and possibly even partially restore vision in individuals with a biallelic mutation in their RPE65 gene, which can present as either retinitis pigmentosa or Leber congenital amaurosis. While the population of patients with this specific mutation is limited, Luxturna’s demonstrated medical efficacy and its successful transformation into a pharmaceutical product underscore the substantial promise of gene therapy in treating various other forms of retinitis pigmentosa moving forward.
Several companies have shifted their focus toward this therapeutic area, and several retinitis pigmentosa therapies are expected to enter the treatment market during our forecast period, including CTx-PDE6b (Coave Therapeutics), AAV5-RPGR (MeiraGTx UK II Ltd) and EA-2353 (Endogena Therapeutics).
Coave Therapeutics is developing CTx-PDE6b, an AAV-based gene therapy designed to deliver a full-length non-mutated copy of the functional human PDE6b gene into the subretinal space, where it rapidly induces robust transgene expression and synthesis of functional PDE6b proteins in photoreceptive rods and cones. By effectively providing these cells with a functional protein, CTx-PDE6b may significantly delay or halt retinal degeneration in PDE6ß-deficient patients. CTx-PDE6b is currently in Phase I/II clinical trials.
AAV5-RPGR is a gene therapy developed by Janssen (Johnson & Johnson) & MEIRAGTx for RPGR-Associated X-Linked Retinitis Pigmentosa. It is delivered via subretinal injection targeting the central retina in the eye that was more affected at baseline. In the recently published results, in a phase I/II study, the gene therapy AAV5-RPGR (MeiraGTx/Janssen) showed positive results in patients with RPGR-associated X-linked retinitis pigmentosa (XLRP). The treatment, delivered via a recombinant adeno-associated virus vector, is also known as botaretigene sparoparvovec.
As per DelveInsight, in the 7MM, the total retinitis pigmentosa market size was estimated to be ~USD 400 million in 2022. Nearly half of this market’s entire revenue came from approved therapies (Luxturna). Moreover, the outlook for retinitis pigmentosa treatments is promising. Various clinical trials for gene therapy and stem cell therapy, have been fairly positive in terms of safety and limited evaluations of efficacy. The results of these studies are encouraging further investigation into the basic physiology of the retina, as well as the mechanisms of effective prevention and reversal of inherited retinal degenerations.

Leber Hereditary Optic Neuropathy (LHON)
Leber’s hereditary optic neuropathy (LHON) represents a unique subset among ‘inherited optic atrophies’ and ‘hereditary optic neuropathies.’ This condition is characterized by optic nerve dysfunction due to point mutations in mitochondrial DNA, and it follows a non-Mendelian pattern of inheritance. LHON is most commonly associated with three mitochondrial base pair mutations: G11778A (guanine to adenine at position 11778), T14484C (tyrosine to cytosine), and G3460A. These mutations predominantly affect genes within respiratory chain complex I, particularly mitochondrial genes ND1, ND4, and ND6, among others. According to the data provided by the American Academy of Ophthalmology, of all the mutations, The G11778A is the most common, reported to account for 70% of cases in Northern European populations and 90% in Asian populations. It is associated with more severe disease, with less chance of significant visual recovery.
At present, Raxone (idebenone) stands as the only drug for LHON treatment within the European Union. However, other therapeutic options are under investigation, including brimonidine, nutritional supplements, and ubiquinone analogs. Additionally, alternative approaches, like the use of steroids and immunosuppressants such as cyclosporine A, are being explored for LHON treatment. One particularly promising avenue lies in the realm of gene therapy.
According to DelveInsight’s estimates, the LHON market in 7MM is expected to show positive growth, during the forecast period (2023–2032), mainly attributed to the anticipated launch of emerging therapies including GS010 – LUMEVOQ (GenSight Biologics), NFS-01 (NR082,rAAV-ND4) (Neurophth), NFS-02 (rAAV-ND1) (Neurophth), and several others, and the increasing cases of LHON.
GS010 is a gene therapy-based single intravitreal injection in the eye targeting LHON. GS010 uses GenSight’s Mitochondrial Targeting Sequence (MTS) proprietary technology platform, which permits missing mitochondrial proteins to be shuttled into the mitochondrion, enabling the restoration of mitochondrial function. It has also received Orphan Drug Designation both in the United States and in Europe. In March 2023, the company announced that efficacy and safety data from patients with LHON carrying the ND4 mutation (ND4-LHON) treated with lenadogene nolparvovec (LUMEVOQ, GS010) through early access programs (EAP), was presented at the 49th Annual Meeting of the North American Neuro-Ophthalmology Society (NANOS). The data was collected from EAPs across the US, France, Italy, and the UK. It is currently evaluated in Phase III of clinical development for LHON treatment.
Neurophth is currently developing two drug candidates for LHON, NFS-01 (NR082, rAAV-ND4) and NFS-02 (rAAV-ND1), to treat LHON diseases caused by G11778A (ND4) site mutation and G3460A(ND1) site mutation, respectively. The mechanism of action is to leverage the gene therapy strategy and use the recombinant adeno-associated virus as the vector to deliver the correct genes to the patient’s damaged optic ganglion cells through Intravitreous injection, thus repairing the mitochondrial biological respiratory chain, and restore the vitality and visual function of optic ganglion cells.

Retinoblastoma
Retinoblastoma is a rare childhood cancer, typically manifesting in children under the age of 5. Approximately 200 to 300 children are diagnosed with retinoblastoma each year. It affects both boys and girls with no gender preference. Most cases involve one eye (unilateral), while about 25% of cases affect both eyes (bilateral). This condition occurs in two primary forms: heritable and non-heritable. The heritable form, which is bilateral, is usually diagnosed at an earlier age. In most cases, retinoblastoma is non-heritable and arises spontaneously without a clear cause.
The treatment of retinoblastoma varies depending on the disease’s stage in each patient. When determining the appropriate treatment strategy, the patient’s healthcare team will take into account whether the cancer is localized within the eye (intraocular retinoblastoma) or has spread to other parts of the body (extraocular retinoblastoma). Various therapeutic approaches are available for retinoblastoma, including local and systemic chemotherapy, cryotherapy, laser photoablation, thermotherapy, radiotherapy, and surgical removal of the affected eye (enucleation).
The current retinoblastoma treatment market anticipates the emergence of emerging retinoblastoma therapies namely VCN-01 (VCN Biosciences), Episcleral Topotecan, and others. VCN-01 by VCN Biosciences is a genetically modified oncolytic adenovirus with unique characteristics being studied in clinical trials for cancers for which there is no cure, including pancreatic carcinoma and refractory retinoblastoma. Recently, in February 2022, VCN-01 was granted the Orphan Drug Designation by the US FDA for the treatment of retinoblastoma. In March 2022, VCN Biosciences was acquired by Synthetic Biologics in order to focus on oncolytic virus development.
Targeted Therapy Technologie’s product Episcleral Topotecan is a semisynthetic derivative of camptothecin, a cytotoxic, quinoline-based alkaloid extracted from the Asian tree Camptotheca acuminata. Topotecan inhibits topoisomerase I activity by stabilizing the topoisomerase I-DNA covalent complexes during the S phase of the cell cycle, thereby inhibiting the religation of topoisomerase I-mediated single-strand DNA breaks and producing potentially lethal double-strand DNA breaks when encountered by the DNA replication machinery. This drug is being studied in Phase I of the clinical trial for the treatment of retinoblastoma patients. In July 2019, the drug received an Orphan Drug Designation from the US FDA. In October 2021, the US FDA granted Breakthrough Therapy Designation to Episcleral Topotecan.
DelveInsight estimated that the retinoblastoma market is anticipated to show positive growth at a significant CAGR by 2032 owing to the increase in the R&D activities and the expected launch of these emerging therapies.
Limbal Stem Cell Deficiency (LSCD)
Limbal stem cell deficiency (LSCD), a condition affecting the ocular surface, arises from a reduction in the population and/or functionality of corneal epithelial stem/progenitor cells. This reduction results in an inability to maintain the standard corneal epithelial equilibrium. The condition is characterized by conjunctivalization, where the normal corneal epithelium is replaced by conjunctival epithelium, as well as other indications of epithelial dysfunction. These may include persistent or recurring epithelial defects, sometimes accompanied by neovascularization, inflammation of the ocular surface, and scarring. DelveInsight estimates that the US accounted for the highest population with Limbal stem cell deficiency (~100K cases) among the 7MM countries in 2021.
Currently, the exclusive medication approved for the treatment of patients with LSCD is HOLOCLAR, which is composed of autologous human corneal epithelial cells containing stem cells. Another option available is OCU-ORAL, which employs human autologous oral mucosa-derived epithelial cell sheets. HOLOCLAR is commercially accessible in European Union countries and is specifically recommended for adult patients with moderate-to-severe LSCD resulting from various causes, including chemical burns to the eyes. This innovative therapy product is categorized as a ’tissue-engineered product, involving the collection of cells from the patient’s limbus, followed by laboratory cultivation to restore the damaged corneal surface.
To cater to the need, many new assets are in the early stage LSCD clinical phase to treat patients across many countries. Some early-stage products that will likely hit the market during our study period (2019–2032) include LSCD101 (CliPS Co., Ltd.) and LSC2 (RHEACELL GmbH & Co. KG), among others.
The limbal stem cell therapy (LSCD101) is a treatment developed by Professor Sohyang Jeong’s team and transferred to CLIPS BnC, the first and only ophthalmic limbal stem cell treatment in Korea. Compared to the autologous limbal stem cell therapy (HOLOCLAR) commercialized in Europe, the limbal stem cell ability is superior to an average of about three times or more, and the safety has been proven as animal-derived cells and culture medium are excluded during cell culture. Currently, a Phase II clinical trial of an autologous limbal stem cell therapy is in progress, and a clinical trial of an allogeneic limbal stem cell therapy is planned for patients with LSCD in both eyes.
DelveInsight’s analysts estimate that the LSCD market is expected to show positive growth and will grow from USD 2.7 billion in 2021 at a significant CAGR by 2032, mainly attributed to increased prevalence and the anticipated launch of novel therapies during the forecast period (2023–2032).

A Glimpse into the Future of Rare Eye Diseases
The future outlook for rare eye diseases holds great promise, thanks to advancements in medical research, technology, and personalized medicine. With innovative treatments and gene therapies, conditions like retinitis pigmentosa, Stargardt disease, and Leber’s congenital amaurosis are poised for transformative change. Gene editing techniques, such as CRISPR, offer the potential to correct genetic mutations responsible for these diseases, potentially restoring vision. Additionally, the advent of artificial intelligence in ophthalmology promises earlier and more accurate diagnosis, while wearable devices and prosthetic implants may provide alternative vision solutions. As we look ahead, the horizon for rare eye diseases is illuminated with hope, offering a brighter future for those who have long endured these debilitating conditions.
Downloads
Article in PDF
Recent Articles
- How the Amniotic Membrane Market is Transforming Regenerative Healthcare Worldwide
- Break the Gene Therapy Barrier with DelveInsight’s Gene Therapy Reports
- Limbal Stem Cell Deficiency (LSCD): A Multifactorial Disease with Challenging Diagnosis and Treat...
- Wainua – The Only Approved Medicine for hATTR-PN Treatment
- Rising of Orphan Drug Development