Advances in Varicose Vein Treatment Devices: Technologies Shaping Modern Venous Care
Jan 28, 2026
Table of Contents
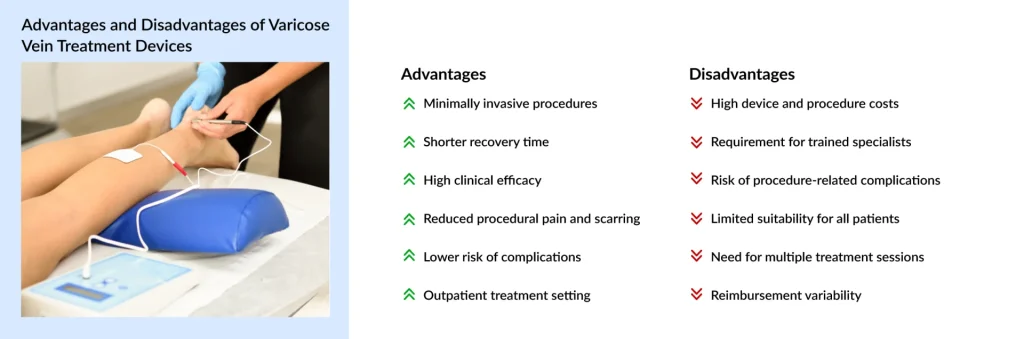
Varicose veins, enlarged, tortuous veins most commonly occurring in the lower extremities, impact millions worldwide, causing discomfort, cosmetic concerns, and, in severe cases, complications such as venous insufficiency or ulcers. While traditional varicose vein treatments such as compression stockings and surgical vein stripping have long been the standard, the last decade has seen a shift in the paradigm. Technological innovation has introduced a suite of minimally invasive devices that are safer, more effective, and significantly more acceptable to patients and clinicians alike. Today’s venous care landscape is defined by precision, reduced downtime, and improved outcomes.
Endovenous Thermal Ablation: The Current Gold Standard
For over two decades, Endovenous Thermal Ablation (EVTA) has stood as the benchmark against which all other varicose vein treatments are measured. By utilizing controlled thermal energy to collapse diseased veins, EVTA has effectively rendered traditional ligation and stripping obsolete.
Downloads
Click Here To Get the Article in PDF
Recent Articles
- Artificial Intelligence in Drug Commercialization: Accelerating Market Success through Data-Drive...
- Medical Radiation Detection Devices: Essential Tools in Healthcare and Diagnostics
- Wireless Brain Sensors: Revolutionizing Neuroscience and Healthcare
- How is Artificial Intelligence (AI) Playing a Constructive Role in Mental Health Management?
- Mobile Clinics: Bridging the Healthcare Gap
Mechanism and Modalities
EVTA primarily encompasses two technologies: Radiofrequency Ablation (RFA) and Endovenous Laser Ablation (EVLA). Both involve percutaneously inserting a thin catheter or laser fiber into the Great Saphenous Vein (GSV) under ultrasound guidance.
Radiofrequency Ablation (RFA): Uses a specialized catheter to deliver heat in 20-second cycles, typically reaching 120°C. This uniform heating causes the vein wall to shrink and seal shut.
Endovenous Laser Ablation (EVLA): Uses laser energy (often at wavelengths of 1470 nm or 1940 nm) to generate steam bubbles that cause targeted thermal damage to the endothelial lining.
Clinical Efficacy
According to clinical registries cited by the CDC and WHO, thermal ablation boasts a technical success rate exceeding 95%. Five-year follow-up data show that approximately 84% of patients remain reflux-free, a stark contrast to the high recurrence rates associated with historical surgical methods. Despite its success, EVTA requires tumescent anesthesia, a series of numbing injections along the leg to create a “heat shield” for surrounding tissues, which remains the primary source of patient discomfort during the procedure.
Non-Thermal Innovations: Medical Adhesive and Foam Technologies
The “Next Generation” of venous care is defined by Non-Thermal, Non-Tumescent (NTNT) technologies. These innovations eliminate the risk of nerve damage from heat and eliminate the need for painful tumescent injections, allowing for a “walk-in, walk-out” experience.
VenaSeal: Medical Adhesive Closure
The VenaSeal Closure System represents a paradigm shift in venous care by utilizing a proprietary, medical-grade adhesive, specifically a formulated cyanoacrylate, to physically seal diseased vein walls together. Unlike the high-heat mechanisms of thermal ablation, VenaSeal operates through a rapid polymerization reaction triggered upon contact with blood, effectively creating a permanent “glue” that collapses the vessel and redirects flow to healthier veins. This innovative approach offers a profound clinical advantage: by eliminating the need for thermal energy, it completely removes the risk of heat-related nerve or skin injury. Furthermore, the procedure avoids the need for tumescent anesthesia and the series of multiple, often painful numbing injections along the leg, allowing for a significantly more comfortable patient experience.
Post-procedural recovery is a cornerstone of the VenaSeal value proposition. Because there is no thermal trauma to the surrounding tissue, patients typically do not need to wear medical-grade compression stockings after the treatment. This is a critical factor in patient compliance, particularly in warmer climates such as Asia and Southern Europe, where heavy hosiery can be prohibitive. The clinical success of this technology is supported by robust data, including the Singapore VenaSeal Study (ASVS), which reported a 100% technical success rate in an Asian patient cohort. Long-term follow-ups from the ASVS and the global VeClose study demonstrate sustained vein closure and significant improvements in quality-of-life scores over 36 months and beyond, confirming VenaSeal as a durable, “walk-in, walk-out” alternative to traditional standards.
Varithena Foam Sclerotherapy
Varithena (polidocanol injectable foam) represents a breakthrough in chemical ablation. Unlike traditional liquid sclerotherapy, which can dilute in the blood, Varithena is a microfoam that displaces blood and ensures uniform contact with the vein wall.
Application: It is particularly effective for tortuous (twisted) veins that are difficult to navigate with a rigid thermal catheter.
Clinical Data: The VERITAS study and other randomized trials have shown that Varithena provides significantly greater symptom relief (assessed via HASTI® scores) than placebo, with a safety profile characterized by only mild, transient adverse events.
Advanced Ultrasound-Guided Technologies
The future of vein treatment is becoming entirely non-invasive through the integration of artificial intelligence and high-intensity focused ultrasound.
High-Intensity Focused Ultrasound (HIFU)
Technologies like the SONOVEIN system are pioneering “extracorporeal” ablation. By focusing ultrasound beams from outside the body to a specific point inside the vein, doctors can seal the vessel without a single needle stick or incision.
2025 Milestones: In December 2025, new clinical trials for the “SpeedPulse” feature showed a substantial increase in treatment speed, making HIFU a commercially viable competitor to traditional ablation in European markets.
AI-Enhanced Diagnostics
Artificial Intelligence is now used to analyze ultrasound images in real time, helping clinicians map “venous twins”, digital models of a patient’s vascular system, to predict the best entry points and energy levels for treatment, thereby minimizing the risk of recurrence.
Varicose Vein Treatment Devices: Market Dynamics and Key Companies
The global varicose vein treatment device market is a highly dynamic sector characterized by moderate concentration and robust growth. According to recent DelveInsight data, the market is expanding at a 6.25% CAGR, reflecting a worldwide shift toward minimally invasive vascular care. At the regional level, North America continues to be the primary engine of the global market, accounting for over 43% of revenue. This sustained leadership is fueled by a high prevalence of obesity-driven venous insufficiency, a well-established network of specialized vein clinics, and a highly favorable reimbursement landscape, particularly for Medicare-covered endovenous thermal ablation.
In contrast, Europe has emerged as the most proactive region in adopting Non-Thermal, Non-Tumescent (NTNT) technologies, such as the VenaSeal closure system. The European market is uniquely supported by a pervasive “office-based” clinic model, particularly in Germany, France, and the UK, which prioritizes rapid, outpatient interventions over hospital-based procedures. Meanwhile, the Asia-Pacific region is projected to be the fastest-growing market globally, with an anticipated CAGR of 7.7%. This rapid acceleration is primarily driven by an expanding geriatric demographic in China and Japan, coupled with rising disposable incomes in India, which are collectively increasing the accessibility and social acceptance of advanced vein treatments.

The competitive landscape of the varicose vein treatment market is increasingly defined by “heavyweight” corporations that leverage aggressive acquisition strategies to consolidate their portfolios and maintain global dominance. Medtronic currently stands at the forefront of this sector, maintaining its leadership position through the widely adopted VenaSeal closure system and the VNUS ClosureFast radiofrequency ablation platform, which remain staples in minimally invasive vein care. Boston Scientific has similarly bolstered its market footprint, most notably through the strategic acquisition of BTG, which brought the innovative Varithena microfoam sclerotherapy system into its vascular portfolio. Meanwhile, AngioDynamics remains a formidable competitor by focusing on a diverse range of endovascular therapies and high-precision laser systems tailored for specialized vein clinics. Complementing these procedural leaders is Teleflex, which secures its market position by supplying high-quality catheter components and vascular access tools essential to the successful execution of these advanced interventions.
Future Outlook: Toward a “Needleless” Era
As we look toward 2032, the trajectory of varicose vein treatment is clear: maximum efficacy with minimum intervention. The convergence of nanotechnology, in which nanobots could potentially repair damaged venous valves, and robotic-assisted vein procedures suggests a future in which human error is minimized. Furthermore, the shift from hospital-based surgeries to Ambulatory Surgical Centers (ASCs) and specialty clinics will continue to drive down costs and improve accessibility.With the global prevalence of venous disorders ranging between 20% and 60% of the adult population, the demand for these advanced devices is not just a cosmetic luxury but a public health necessity. The ongoing transition from thermal to non-thermal, and eventually to non-invasive ultrasound, ensures that the “gold standard” will continue to evolve in favor of the patient.
Downloads
Article in PDF
Recent Articles
- The Automated Eye: How AI-Driven Diagnostics are Reshaping the Future of Medical Imaging
- Artificial Intelligence (AI) in Respiratory Care: An Opportune Time for Adoption in Clinical Sett...
- Understanding How Emerging Applications of Nanotechnology are Upgrading the Healthcare Delivery?
- Baird Medical’s Microwave Ablation System; BrainSpec’s AI-Backed Solution for Non-Invasive Brain ...
- Nanomedicine’s Impact: Transforming the Future of Healthcare Industry Dynamics