The Future of Pain Management Devices: AI and Digital Integration
Feb 11, 2026
Table of Contents
The convergence of artificial intelligence and connected health technologies is fundamentally transforming chronic pain management, shifting from reactive treatment protocols to proactive, personalized care systems. This integration represents not merely an incremental improvement but a paradigm shift in how patients experience and manage persistent pain conditions.
The Convergence of AI and Pain Management: A New Paradigm
Traditional pain management has relied heavily on patient-reported outcomes and fixed therapeutic protocols, often resulting in suboptimal treatment efficacy. The integration of artificial intelligence into pain management devices is revolutionizing this approach by enabling real-time adaptation, predictive analytics, and personalized therapy delivery. AI algorithms now analyze physiological data, including evoked compound action potentials (ECAPs), facial expressions, sleep patterns, and activity levels, to continuously optimize treatment parameters without requiring constant clinical intervention.
Downloads
Click Here To Get the Article in PDF
Recent Articles
- ONWARD Medical’s ARC-EX System Gains CE Mark; Microbot Medical Secures FDA 510(k) Clearance for L...
- JPM 2026 Recap: Who’s Winning, Who’s Catching Up, and Who’s at Risk?
- The AI Drug Discovery Revolution: Smarter Science, Faster Therapies, Better Outcomes
- 22 Healthcare Trends & Innovations to Watch in 2022 and Beyond
- Snippet
This technological convergence addresses critical limitations of conventional therapies, including inconsistent patient outcomes, challenges in patient selection, and difficulties sustaining therapeutic efficacy over time. By embedding machine learning directly into therapeutic devices, manufacturers are creating intelligent systems that learn from patient responses and automatically adjust stimulation patterns to maintain optimal pain relief.
Market Growth: Explosive Expansion of Smart Pain Management Solutions
The pain management devices market is experiencing robust growth driven by technological innovation and the global shift away from opioid-based treatments. The global market is expected to grow from USD 5.2 billion in 2024 to USD 9.3 billion by 2032, reflecting a 7.53% CAGR.
Neurostimulation devices continue to dominate the pain management market, accounting for 43.6% of the market share in 2024. Within this segment, spinal cord stimulators (SCS) constitute the largest category, accounting for more than 45% of the neurostimulation market in 2024.
The leading companies operating in the pain management devices market include Abbott Laboratories, Smith’s Medical, B. Braun SE, Baxter International, Boston Scientific Corp., Avanos Medical, Inc., Medtronic, Nevro Corp., ICU Medical, Inc., Omron Corporation, Stimwave LLC, Nipro, O&M Halyard, EndoStim Inc., Nalu Medical, Inc., Micrel Medical Devices SA, DyAnsys, Inc., NanoVibronix, Inc., Zynex Inc., and others.

Advanced Technologies Revolutionizing Pain Assessment and Management
The technological evolution in pain management spans multiple domains, from implantable neurostimulators to wearable sensors and cloud-based analytics platforms. These innovations share common characteristics: wireless connectivity, AI-driven personalization, closed-loop feedback mechanisms, and integration with broader digital health ecosystems.
Wireless Ultrasound-Induced Implantable Stimulators: The Next Generation
A breakthrough innovation emerging from research at USC Viterbi’s Alfred E. Mann Department of Biomedical Engineering and UCLA represents a significant leap forward in implantable pain management technology. The Ultrasound-Induced Wireless Implantable (UIWI) stimulator eliminates the need for bulky batteries and complex wired interfaces, which typically require repeated surgical interventions.
Technical Architecture
The UIWI stimulator operates through a sophisticated energy conversion system:
- Power Delivery: Receives energy from an external wearable ultrasound transmitter (WUT), utilizing ultrasound’s safe, non-invasive deep-tissue penetration capabilities
- Energy Conversion: Converts mechanical waves into electrical signals through the piezoelectric effect using a miniaturized lead zirconate titanate (PZT) element
- Form Factor: Flexible design that bends and twists with patient movement, secured directly to the spine
- Closed-Loop Control: Automatically adjusts acoustic energy transmission based on real-time pain level detection, creating a self-adaptive pain management system
This wireless power approach addresses critical limitations of conventional implantable stimulators, including the need for replacement surgeries, device corrosion, and scar tissue accumulation around electrodes.
Closed-Loop Spinal Cord Stimulation: Precision Pain Control
Closed-loop spinal cord stimulation is at the forefront of precision pain management, using real-time physiological feedback to dynamically optimize therapy delivery. Unlike traditional open-loop systems that deliver fixed stimulation patterns, closed-loop systems continuously monitor neural responses and automatically adjust parameters to maintain therapeutic efficacy.
Key Closed-Loop Systems
Nevro HFX AdaptivAI: Launched in September 2024, this FDA-cleared system represents the first AI-driven spinal cord stimulation platform that uses real-time patient data to personalize and optimize therapy. The system aims to deliver more consistent, effective pain relief by adapting to patient needs in real time.
Medtronic Inceptiv: FDA-approved in April 2024, this closed-loop, rechargeable SCS system automatically adjusts stimulation based on real-time biological feedback from evoked compound action potentials (ECAPs). It maintains optimal therapy even during patient movement and is the only FDA-approved closed-loop system that provides unrestricted access to full-body 3T MRI.
Boston Scientific AI-Driven Recommender: Developed in partnership with IBM Research, this system uses “Patient States”, a comprehensive measure of well-being including sleep, activity, mood, and medication use, to optimize therapy recommendations. Early results demonstrate improvements in patient state dwell time for more than half of SCS patients, many of whom previously experienced suboptimal outcomes.
These systems demonstrate significant clinical advantages, including sustained pain relief, reduced programming burden, improved device longevity, and higher response rates enabled by predictive modeling for patient selection.
AI-Driven Wearable Systems: The NXTSTIM EcoAI Platform
The NXTSTIM EcoAI platform exemplifies how artificial intelligence is transforming non-invasive pain management. This FDA-approved wearable device combines transcutaneous electrical nerve stimulation (TENS) with electromyographic sensing to deliver personalized neuromodulation therapy.
Clinical Validation
- An 18-month real-world study involving 550 adult patients demonstrated compelling efficacy:
- 92% of patients reported pain improvement compared to baseline
- 66% exhibited at least 40% improvement on the visual analogue pain scale
- Pain sites included back, neck, shoulder, and knee conditions
Technical Features
The EcoAI device works by blocking pain signals from the peripheral nervous system to the central nervous system. Key capabilities include:
- Pre-configured stimulation programs based on historical clinical evidence
- AI algorithms that record patient data and generate individualized neurostimulation programs
- Bluetooth connectivity enables smartphone-based device control
- Gel pad application for targeted pain site treatment
This platform demonstrates how AI-enabled wearables can bridge the gap between clinical intervention and at-home pain management, providing continuous personalized therapy without requiring frequent clinical visits.
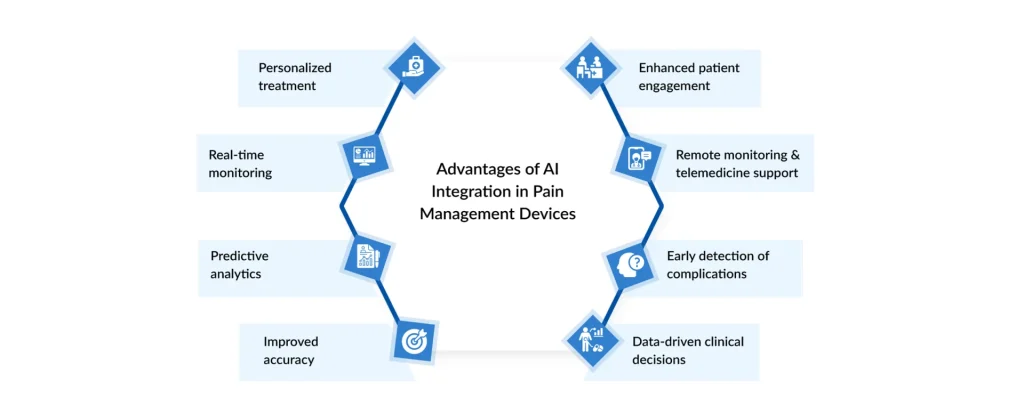
Integration with Digital Health Platforms: Enabling Remote Monitoring and Personalization
The integration of pain management devices with comprehensive digital health platforms is enabling a shift toward remote patient monitoring and data-driven care coordination. This ecosystem connects patients, devices, and healthcare providers through seamless data flow, creating opportunities for proactive intervention and personalized treatment optimization.
Internet of Things (IoT) Architecture
Modern IoT-based pain management systems employ sophisticated multi-layer architectures that enable real-time monitoring and automated pain assessment:
Sensor Layer
Wearable devices function as wireless sensor nodes that sample multiple physiological channels at high frequencies (up to 1000 Hz for sEMG). These sensors capture comprehensive biometric data, including surface electromyography, movement patterns, and physiological indicators of pain states.
Connectivity Layer
Bluetooth Low Energy (BLE) technology enables seamless communication between wearable devices and mobile applications while maintaining low power consumption for extended use. More advanced systems incorporate gateway devices that bridge local sensor networks with cloud infrastructure.
Cloud Platform Layer
Cloud-based platforms serve as central hubs managing wireless communication between sensor nodes and end-user applications. These platforms handle high-volume data streaming, digital signal processing, and secure data storage while maintaining HIPAA compliance.
Application Layer
Mobile web applications provide real-time data visualization, treatment-control interfaces, and patient-engagement tools. These applications enable remote monitoring for caregivers while giving patients direct control over their therapy parameters.
Mobile Application Integration and Patient Engagement
Mobile applications have become essential components of modern pain management ecosystems, serving as both patient engagement tools and clinical interfaces. These applications provide:
- Real-time device control: Wireless adjustment of stimulation parameters, intensity levels, and treatment programs
- Treatment adherence support: Automated reminders, therapy session tracking, and progress visualization
- Patient feedback collection: Structured pain assessment tools, symptom tracking, and quality-of-life metrics
- Long-term treatment planning: Historical data analysis and trend identification to optimize therapeutic approaches
The integration of intuitive user interfaces for both patients and healthcare providers ensures that sophisticated AI-driven therapy remains accessible and manageable for diverse user populations.
Cloud-Based Analytics and Predictive Intelligence
Cloud-based analytics platforms transform raw biometric data into actionable clinical insights through advanced processing capabilities:
Predictive Analytics
Machine learning algorithms analyze historical pain patterns, medication usage, activity levels, and sleep quality to predict pain flare-ups before they occur. This predictive capability enables timely intervention and proactive adjustments to therapy.
AI-Driven Treatment Optimization
Cloud-based AI systems continuously refine treatment algorithms based on aggregated patient data. These systems combine on-device inference for real-time adjustments with cloud-based learning to improve therapeutic models across patient populations.
Population Health Insights
Aggregated data from connected pain management devices enables researchers and healthcare systems to identify broader patterns in the efficacy of chronic pain treatments, informing evidence-based protocol development and resource allocation strategies.
Security and Compliance
Modern cloud architectures implement end-to-end encryption and stringent access controls to protect sensitive health information. Compliance with medical-grade security standards ensures patient privacy while enabling data sharing necessary for collaborative care.
Conclusion: A Paradigm Shift in Pain Management
The integration of artificial intelligence and digital connectivity into pain management devices represents a fundamental transformation in chronic pain care. From wireless, ultrasound-powered implants that eliminate the need for battery replacement surgeries to AI-driven closed-loop systems that continuously optimize therapy delivery, these technologies are addressing long-standing limitations of conventional pain management.
The market trajectory reflects this transformation, with AI-powered pain management solutions experiencing explosive growth, outpacing growth in traditional medical device segments. As these technologies mature, we can anticipate continued convergence of implantable and wearable solutions, increasingly sophisticated predictive algorithms, and deeper integration with comprehensive digital health ecosystems.For the millions of patients worldwide living with chronic pain, these innovations promise not merely incremental improvements in symptom management but a fundamentally enhanced quality of life through personalized, adaptive, and data-driven care. The future of pain management is intelligent, connected, and patient-centered, a paradigm that puts real-time therapeutic optimization within reach for every individual managing persistent pain.
Downloads
Article in PDF
Recent Articles
- From Lab to Bedside: The Rise of AI-Enabled Digital Pathology
- Mainstay Medical’s ReActiv8-C Study; Swing Therapeutics Announced Results from Studies of S...
- Johnson & Johnson MedTech Secures CE Mark for Dual Energy THERMOCOOL SMARTTOUCH™ SF Catheter;...
- FDA Clears Stryker’s Incompass Total Ankle System; Glaukos Receives EU MDR Approval for iStent in...
- Noninvasix’s LIVOx™ Central Venous Oxygenation Monitor; LivaNova’s aura6000 System; Oxford...