Late-Breaking Science at AAN 2025: Shaping the Future of Neurology
Apr 25, 2025
Table of Contents
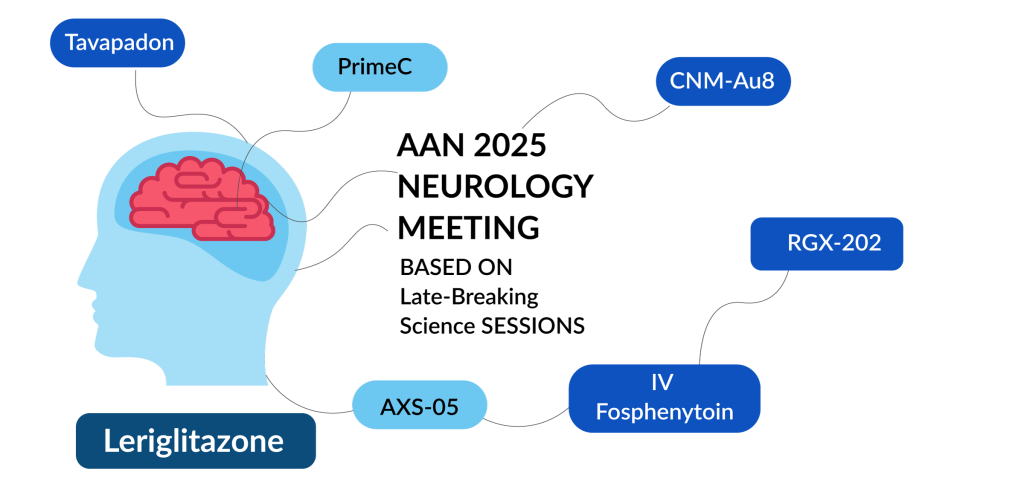
The 77th Annual Meeting of the American Academy of Neurology (AAN 2025), held from April 5–9 in San Diego and online, served as a pivotal forum for advancing research in neurology, with particular relevance to neurodegenerative diseases. As one of the largest gatherings of neurologists globally, the conference provided a critical platform for unveiling new data, fostering cross-disciplinary collaboration, and translating scientific discoveries into clinical strategies.
For the neurodegenerative disease field—spanning Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, and others—AAN 2025 delivered high-impact presentations that addressed gaps in diagnosis, therapeutic development, and disease management. The inclusion of over 3,200 scientific abstracts highlighted the fast-paced advancements in the field, while the participation of over 14,500 attendees from 110 countries underscored the growing urgency and global relevance of these issues.
Downloads
Click Here To Get the Article in PDF
Recent Articles
- Enhancing Patient Care: Transitioning from Eculizumab to Ravulizumab in gMG Management
- Prothena’s Promise: Revolutionizing Alzheimer’s Treatment with a Breakthrough Therapy
- Transforming Rapid Seizure Termination Care with STACCATO Alprazolam
- Navigating the Emerging Trends and Technologies in the Spinal Cord Injury Rehabilitation Segment
- From Wrist to Wellness: The Evolving Landscape of Wearable Medical Devices Market
Late-breaking abstracts were particularly emphasized, highlighting emerging treatments and breakthrough findings that were too recent for the regular submission timeline. These presentations often featured the first disclosures of Phase II or Phase III trial data, novel drug mechanisms, or biomarker validation—developments that can influence clinical practice and regulatory pathways.
In this context, AAN 2025 functioned not just as a scientific meeting but as a catalyst for progress in addressing the unmet needs in neurodegenerative disease care and innovation.
Late-breaking Science 1
AbbVie’s Dual TEMPO Trials Validate Tavapadon’s Monotherapy Potential
At AAN 2025, AbbVie presented late-breaking results from its Phase III TEMPO-2 and TEMPO-1 trials, evaluating tavapadon, a once-daily oral selective D1/D5 partial dopamine agonist, for early Parkinson’s disease.
The TEMPO-2 trial offered the first Phase III evidence of tavapadon’s efficacy using a flexible-dose regimen, demonstrating a statistically significant improvement in combined motor and functional scores (MDS-UPDRS Part II+III, LSM difference: –9.1) compared with placebo. The findings suggest that tavapadon may deliver clinically meaningful benefits while maintaining a favorable safety profile, with most adverse events being mild to moderate.
Similarly, the TEMPO-1 trial assessed fixed doses (5 mg and 15 mg), both of which yielded significant improvements in MDS-UPDRS Part II+III scores (–11.5 and –12.1, respectively). The improvement in daily function scores further supports symptom control and potential dose-related therapeutic impact.
Both studies reinforce the clinical relevance of selective D1/D5 receptor targeting, distinguishing tavapadon from conventional D2/D3-based therapies. These data position tavapadon as a promising monotherapy option in early Parkinson’s disease, potentially reshaping the treatment paradigm.
Analyst’s Views: “Tavapadon, AbbVie’s once-daily, selective D1/D5 partial dopamine agonist, demonstrated clinically meaningful improvements in motor function in early Parkinson’s disease, as shown in the TEMPO-1 and TEMPO-2 trials presented at AAN 2025. Both fixed and flexible dosing regimens led to symptom relief within the first month, with a safety profile superior to that of traditional dopaminergic agents. Notably, flexible-dose tavapadon in TEMPO-2 showed sustained efficacy and tolerability, reinforcing its potential as monotherapy in early Parkinson’s disease. AbbVie’s ongoing open-label TEMPO-4 trial will further assess long-term outcomes, while data from adjunctive therapy studies (TEMPO-3) broaden its applicability across disease stages. With a New Drug Application (NDA) planned for 2025, the company anticipates regulatory approval for Tavapadon in Parkinson’s disease by 2026. Around 1.2 million people in the US were diagnosed with Parkinson’s disease in 2024, reflecting an increasing healthcare challenge, as per DelveInsight’s Parkinson’s Disease Epidem-based Market Report. Within this landscape, Tavapadon’s unique mechanism of action presents a compelling opportunity to address existing treatment gaps in early-stage Parkinson’s care.”
AXS-05 Slows Agitation Relapse in Alzheimer’s with no Cognitive Decline
In the Phase III ACCORD-2 trial, AXS-05 (dextromethorphan-bupropion) demonstrated clinical efficacy and safety in managing agitation associated with Alzheimer’s disease. Among 167 responders during the open-label phase, AXS-05 significantly delayed time to agitation relapse (hazard ratio = 0.276) and reduced relapse rates (8.4% vs. 28.6%) during the 26-week randomized withdrawal phase. It also prevented the worsening of overall clinical status and agitation severity. Adverse event rates were comparable between AXS-05 and placebo, with low discontinuation and no evidence of sedation or cognitive decline. These findings support AXS-05 as a well-tolerated and effective therapy for agitation in Alzheimer’s disease.
Analyst’s Views: “Axsome Therapeutics’ AXS-05 offers a promising, innovative approach to treating Alzheimer’s disease agitation, a condition affecting 70% of Alzheimer’s disease patients—with limited FDA-approved treatment options currently available. Data from the ACCORD-2 trial demonstrate AXS-05’s efficacy in reducing Alzheimer’s disease agitation without increasing mortality, falls, sedation, or cognitive decline. This is particularly relevant given the substantial disease burden of the disease. DelveInsight estimates indicate that in 2024, approximately 16 million individuals were diagnosed with Alzheimer’s disease across the 7MM, with the US representing 45% of cases and the EU4, plus the UK, contributing close to 30%. Additionally, as per the company’s projections, AXS-05 is estimated to reach peak sales of USD 1.5–3 billion, primarily driven by its potential in treating Alzheimer’s disease agitation. Despite the data not being entirely novel, its first high-profile presentation at AAN 2025 underscores the significant potential of AXS-05 to address this critical unmet need. Backed by favorable data and an NDA submission expected by late 2025, the drug is on track for regulatory review, reinforcing its commercial promise within the neuropsychiatric space.”
Currently, there is only 1 approved drug for treating agitation in Alzheimer’s disease; however, there are a few in the pipeline, as shown in the table below:
IV Fosphenytoin Emerges as the First Non-Surgical Relief for Acute Trigeminal Neuralgia
According to late-breaking findings from the IFT Study presented at the 2025 AAN Meeting, IV Fosphenytoin (fPHT) showed rapid and significant pain relief for acute trigeminal neuralgia flares. In this Phase III trial involving 21 patients, fPHT led to a notable reduction in pain scores within 120 minutes compared to placebo, with 90.9% experiencing at least a 50% improvement versus 40.0% with placebo. fPHT also reduced the frequency of pain episodes between doses. Reported side effects were mild to moderate. These results support fPHT as a potential emergency treatment for refractory trigeminal neuralgia.
Analyst’s Views: “The IFT Study is the first Phase III trial evaluating intravenous fosphenytoin for acute trigeminal neuralgia exacerbations, a critical, painful condition often resistant to oral therapies. The study’s recent data suggest IV fosphenytoin as a fast-acting, well-tolerated alternative to invasive procedures like microvascular decompression. Its clinical relevance and novelty make it a potential practice-changing option, addressing a significant treatment gap. With further development expected, including Nobel Pharma’s partnership with Pfizer for a Phase III trial of fosphenytoin (NPC-06), a breakthrough in acute trigeminal neuralgia management may be possible by 2026.”
Early Efficacy of ALMB-0166 Shows Promise in Acute Spinal Cord Injury (SCI)
In a multicenter Phase I/II trial, ALMB-0166, a first-in-class monoclonal antibody targeting connexin-43 hemichannels, showed favorable safety and early efficacy signals in acute SCI. Among 24 patients treated within 72 h of injury, treatment-emergent adverse events were comparable between ALMB-0166 and placebo, with fewer severe events in the ALMB-0166 group. By day 56, ALMB-0166 was associated with greater improvements in motor and sensory scores, AIS grade recovery, and pain reduction vs. placebo. No deaths occurred. These findings suggest ALMB-0166 may offer a novel neuroprotective approach for acute SCI, warranting further investigation in larger trials.
Analyst’s Views: “ALMB-0166 offers a novel, first-in-class approach to treating SCI by targeting secondary injury mechanisms, specifically inhibiting connexin-43 hemichannels in astrocytes. This mechanism reduces inflammation, excitotoxicity, and axonal degeneration, promoting neurological recovery. With a strong safety profile and the FDA’s Orphan Drug Designation (ODD), ALMB-0166 has the potential to address significant unmet needs in spinal cord injury treatment. By focusing on neuroprotective pathways rather than just symptom management, it may improve long-term outcomes for patients facing limited recovery options after acute SCI.”
Late-breaking Science 2
Phase III Trial Confirms Telitacicept Benefit in Myasthenia Gravis
At AAN 2025, Alexion presented phase III results evaluating telitacicept in generalized myasthenia gravis, targeting B cell–mediated pathology via inhibition of B Lymphocyte Stimulator (BLyS) and a proliferation-inducing ligand (APRIL). In 114 randomized patients, telitacicept significantly improved MG-ADL (–6.4 vs. –1.6) and QMG (–7.8 vs. –1.9) at Week 24 compared to placebo. Secondary endpoints, including QMG and responder rates, also favored telitacicept, with 98.1% achieving ≥3-point MG-ADL and 87.0% achieving ≥5-point QMG reduction, vs. 12.0% and 16.0% on placebo. Immunoglobulin levels (IgG, IgA, and IgM) declined as expected; IgM reduction was the most common AE. The safety profile was consistent with previous data. An open-label extension is ongoing to evaluate long-term outcomes.
Analyst’s Views: “Telitacicept’s dual inhibition of BLyS and APRIL offers a targeted approach to treating generalized myasthenia gravis by directly addressing B-cell-driven autoimmunity. Phase III data have reinforced its efficacy, highlighting its potential as a disease-modifying therapy. With nearly all patients showing significant symptom improvement, telitacicept could transform treatment strategies in a field where durable options are scarce. Additionally, its established presence in the European market since 2022 for treating Systemic Lupus Erythematosus (SLE) provides a strong foundation for broader acceptance among patients, enhancing its potential adoption for myasthenia gravis and expanding its utility in autoimmune diseases driven by B-cell dysregulation.”
VISIONARY-MS Extension Links CNM-Au8 to Neuronal Repair
The long-term results from the Phase II VISIONARY-MS open-label extension provided compelling evidence of remyelination and neuronal repair with CNM-Au8, an investigational metabolic enhancer in multiple sclerosis. Over 144 weeks, improvements in Visual Evoked Potential (VEP) latency—indicating enhanced conduction—correlated with functional gains in vision (LCLA, r = –0.35) and cognition (SDMT, r = –0.34). Anatomical markers of remyelination, including magnetization transfer ratio (MTR) and axonal diffusivity (AD), also correlated with improved VEP measures (e.g., AD and latency, r = –0.41; AD and amplitude, r = 0.45). The strong correlation between MTR and AD (r = 0.746) reinforces the interpretation of structural recovery. These findings represent the first phase II clinical trial evidence linking MRI and physiological biomarkers with meaningful clinical outcomes in multiple sclerosis, suggesting that CNM-Au8 may promote endogenous remyelination. The data signal a potential shift in multiple sclerosis treatment from symptom management toward repair-focused neurotherapeutics.
Analyst’s Views: “CNM-Au8 represents a promising step forward in remyelination therapy for multiple sclerosis, addressing a longstanding unmet need. Unlike previous attempts at remyelination, CNM-Au8’s mechanism of action—enhancing cellular energy metabolism via catalytically active gold nanocrystals—has demonstrated both clinical improvement and evidence of tissue repair in the VISIONARY-MS trial. These results, linking improved MRI and VEP measures to enhanced clinical outcomes, mark a significant advancement in multiple sclerosis therapeutics. Additionally, in 2025, critical milestones for multiple sclerosis include the FDA End-of-Phase II (EOP2) meeting, global Phase III trial protocol alignment, and REPAIR-MS Phase II readout targeting non-active progressive multiple sclerosis. The ongoing expanded access program and the upcoming Phase III trial will be critical in confirming CNM-Au8’s potential as a disease-modifying treatment in multiple sclerosis and other neurodegenerative diseases.”
PrimeC Shows Biomarker and Functional Impact in Amyotrophic Lateral Sclerosis (ALS) Phase IIb Trial
Late-breaking data from the Phase IIb PARADIGM trial support PrimeC’s multimodal mechanism in ALS, showing meaningful target engagement through modulation of miRNA expression and iron metabolism. PrimeC significantly altered over 100 miRNAs, including the downregulation of hsa-miR-199a-5p, an ALS progression marker, and influenced miRNA maturation pathways. It also improved iron biomarkers, notably reducing ferritin and trending toward increased transferrin. Clinically, PrimeC slowed functional decline by 32.8% and showed a 58% survival benefit trend. These findings indicate a mechanistic and clinical signal of efficacy, positioning PrimeC as a promising disease-modifying therapy, with Phase III development well justified.
Analyst’s Views: “NeuroSense’s Phase IIb PARADIGM data provide a compelling mechanistic and clinical validation for PrimeC in ALS. The consistent modulation of over 100 disease-relevant microRNAs, including key regulators of neuroinflammation and iron metabolism, highlights robust target engagement—a longstanding challenge in ALS drug development. These findings signal meaningful therapeutic potential when coupled with a 32.8% slowing in disease progression and favorable safety. Importantly, ODD from both the FDA and EMA, alongside positive alignment in a Type C FDA meeting, de-risks the regulatory strategy. With Phase III initiation set for mid-2025, PrimeC is positioned as a differentiated, mechanism-driven candidate in a high-unmet-need space.”
First-in-Class Micro Dystrophin With C-terminal Domain Shows Functional Gains in Duchenne Muscular Dystrophy (DMD)
Interim data from the AFFINITY DUCHENNE trial highlight RGX-202 as a promising one-time gene therapy candidate for DMD. RGX-202 is unique in encoding a micro dystrophin that retains the C-terminal domain, a region critical for muscle repair and resilience. Among 11 boys aged 1–11 years, RGX-202 demonstrated dose-dependent, robust micro dystrophin expression (10.4–83.4% at DL1; 20.8–77.2% at DL2) and favorable safety with no serious AEs. Early functional data suggest clinically meaningful improvements in NSAA and time function tests, exceeding age- and function-matched external natural history controls. These findings provide strong preliminary evidence of target engagement and therapeutic effect. The CT domain’s inclusion could differentiate RGX-202 from other gene therapies by offering greater durability of muscle protection. As enrollment progresses, longer-term data will be critical to assess sustained efficacy, but these interim results position RGX-202 as a potentially transformative therapy in the high-need DMD landscape.
Analyst’s Views: “RGX-202 emerges as a differentiated next-generation gene therapy candidate in DMD, with interim Phase I/II data indicating robust micro-dystrophin expression and measurable functional improvement on NSAA at both DL1 and DL2 dose levels. The therapy exceeded natural history controls despite limited follow-up, underscoring early signs of disease modification. With pivotal Phase III enrollment expected to be completed in the second half of 2026 and a BLA submission anticipated in mid-2026 via the accelerated approval pathway, RGX-202 is positioned for a potential 2027 launch. The therapy addresses a high unmet need, as only one gene therapy is currently approved for Duchenne. Regenxbio’s broad label strategy and concurrent AFFINITY BEYOND screening study for AAV8 seroprevalence could expand patient eligibility, offering a differentiated path in a market with limited durable therapeutic options.”
Pediatric Cerebral Adrenoleukodystrophy (cALD) NEXUS Program Achieves Regulatory Momentum for Leriglitazone
The NEXUS Phase II/III trial of leriglitazone in boys with childhood cALD demonstrated a clinically meaningful disease-arrest effect in 35% of patients (7 of 20), significantly exceeding the 10% arrest rate observed in natural history data. Disease arrest was defined by stable neurological function, absence of major functional disabilities, and no MRI lesion progression over 96 weeks. All patients remained MFD-free, with no serious TRAEs or discontinuations, underscoring a favorable safety profile. As a once-daily oral therapy, leriglitazone represents a non-invasive alternative to hematopoietic stem cell transplant, potentially enabling earlier intervention upon lesion detection. These findings validate peroxisome proliferator-activated receptor γ modulation as a disease-modifying strategy for cALD and highlight leriglitazone’s promise in addressing a high unmet need in this rapidly progressive, life-threatening pediatric condition. Further insights from secondary and exploratory endpoints may strengthen its case for regulatory advancement.
Analyst’s Views: “Minoryx Therapeutics’ lead PPARγ agonist, leriglitazone, has shown promising clinical and regulatory progress in the treatment of cALD. The Phase II/III NEXUS trial met its primary endpoint, demonstrating clinical stability and radiological disease arrest in pediatric cALD patients at 96 weeks, surpassing the 10% benchmark from natural history data. The earlier 24-week data also indicated stable disease with lesion stabilization. In parallel, the ADVANCE trial in adults with X-ALD revealed reduced cerebral lesion progression. With the ongoing CALYX trial for progressive adult cALD and the positive NEXUS trial outcomes, Minoryx and Neuraxpharm are preparing for a European Marketing Authorization Application (MAA) submission by mid-2025. Leriglitazone’s strong clinical efficacy positions it as a differentiated, first-in-class CNS therapy with significant potential across both pediatric and adult cALD populations.”

Downloads
Article in PDF
Recent Articles
- Top 12 Most Expensive Drugs in the US Healthcare Market
- Amylyx’s AMX0114 Fast Tracked by FDA for ALS; Cellectar’s Iopofosine I 131 Granted FDA Breakthrou...
- Takeda and AC Immune’s Alzheimer’s Deal; Eli Lilly’s Donanemab FDA Review; Bristol Myers Sq...
- Comprehensive Insights into Ocrelizumab: From Early-stage RRMS to Long-term Treatment and Subcuta...
- Tetra, Shionogi sign deal; Amgen remunerates; Gilead’s fibrotic disease deal