Minimal Residual Disease (MRD) Testing: A Path to Cure Cancer?
Feb 27, 2023
Table of Contents
Measurable or Minimal Residual Disease (MRD) is a term often used when treating patients with blood cancers. MRD is a small number of cancer cells left in the body after cancer treatment, and these cells can potentially cause relapse in these patients. The number of remaining cells is often too small to cause any signs or symptoms, and the number is too small even to be detected through traditional methods, such as complete blood counts or tracking serum proteins in the blood. Minimal Residual Disease can be found only by highly sensitive laboratory methods that can find one cancer cell among 1 million normal cells. Checking to see if there is Minimal Residual Disease may help plan treatment, determine how well treatment is working, or make a prognosis.
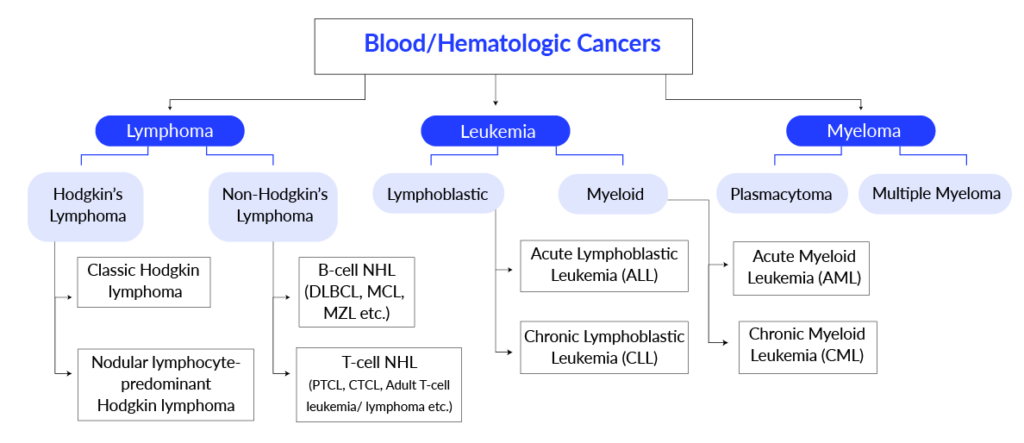
Minimal Residual Disease testing is mainly used in blood cancers but is being studied in other cancers as well. Leukemia, lymphoma, and myeloma are some of the most common types of blood cancer, and some other types are not as common, like Myeloproliferative neoplasms (MPN) and Myelodysplastic syndromes (MDS).Many types of options can be used for the treatment of blood cancers. The type of cancer treatment a patient will undergo depends on the type of cancer and how advanced it is; however, because of blood cancers’ rapid growth, most patients need to start chemotherapy soon after diagnosis.
Downloads
Click Here To Get the Article in PDF
Recent Articles
- Cilta-Cel’s Prolonged Impact: Deep Responses and Safety Insights from Earlier Lines of Ther...
- The Promise of NK Cells: A Novel Approach to Immunotherapy
- Notizia
- CEPI Grants $41.3 Million to Valneva; Innovent Achieves Phase III Success for Mazdutide; GSK’s BL...
- Leo Pharma’s Hand Eczema Clinical Trial Updates; GSK’s PD-1 inhibitor Jemperli Approval; Ro...
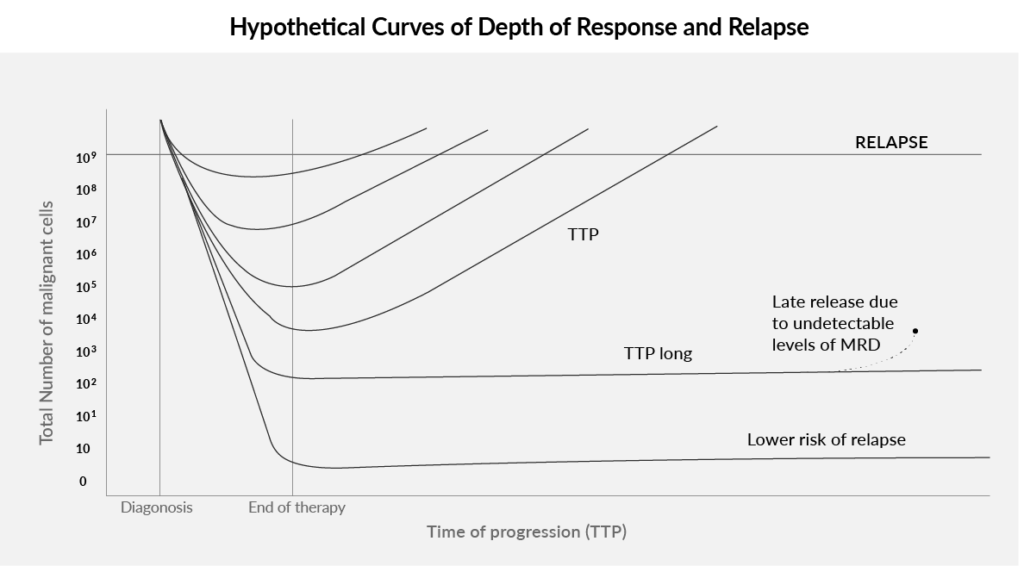
In the treatment of blood cancers, the first phase of cancer treatment is called induction therapy. The goal of induction therapy is to destroy as many cancer cells as possible to achieve (induce) remission. Even when complete remission is achieved, some cancer cells that cannot be seen with a microscope may remain in the body (MRD+). Patients who have achieved remission after initial cancer treatment but have MRD are at increased risk of disease relapse.
After achieving CR, consolidation therapy is the next cancer treatment phase. Consolidation chemotherapy is administered after the initial treatment to target cancer cells that may still be in the body. As in the post-transplant setting, the goal of consolidation for non-transplant patients is to deepen and consolidate the gains made with the initial cycles of therapy. After consolidation, the next phase includes giving maintenance therapy to help prevent cancer from returning after it has disappeared following the initial therapy. It may include cancer treatment with drugs, vaccines, or antibodies that kill cancer cells and may be given for a long time.
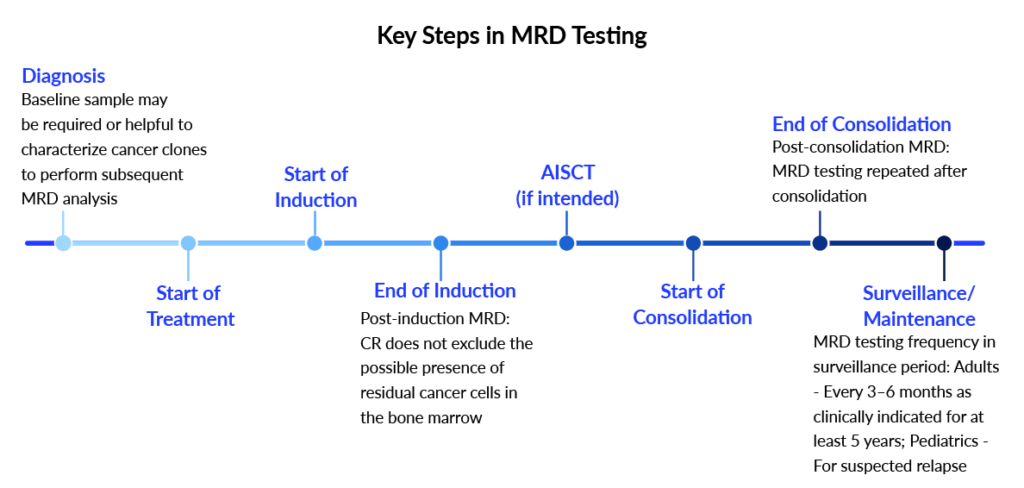
It is important to get tested for Minimal Residual Disease after achieving remission. Flow cytometry, polymerase chain reaction (PCR), and next-generation sequencing are often used to detect MRD. These three MRD tests typically use samples of bone marrow cells, but in some cases, blood samples can be used. The tests are much more sensitive than standard tests that examine cell samples with a microscope. It is often recommended that MRD testing be done after the completion of induction therapy. Recommendations for additional MRD testing depend on the treatment regimen used. An MRD positive test result means that residual (remaining) disease was detected. A negative result means residual disease was not detected, and no cancers were found. This means no more cancer is left in the body, and the cancer treatment has been effective. For Acute Lymphoblastic Leukemia patients in remission who test positive for MRD, blinatumomab (Blincyto) may be prescribed.
Even though MRD detection is necessary, the specific measurement mechanism profoundly affects analytical sensitivity, with different methods having limits of detection ranging over several logs. This assay-sensitivity dependence, and the recognition that a negative test does not imply the absence of disease, is the primary reason why the field has shifted from the term “minimal residual disease” to “measurable residual disease” in the last few years.
Impact of MRD assessment in patient care
MRD testing offers a high-sensitivity evaluation which helps physicians at many levels during the cancer treatment course like, MRD testing during the cancer treatment highlights how effective the cancer treatment is to the patient, is patient resistant to the given therapy or not. This helps physicians to make critical decisions like whether to continue the same course of cancer treatment or change the intensity, or should change the therapy itself depending upon the MRD results. MRD testing after completion of cancer treatment helps to detect the risk of relapse. For example, patients treated for mantle cell lymphoma and achieving an MRD-negative status have been shown to have prolonged remissions before their disease progresses.
MRD is not a surrogate marker for detecting cancer cells but rather a direct measure of them. MRD has quickly become an essential measurement in assessing response in patients with multiple myeloma, as evidenced by its incorporation into the IMWG 2016 response criteria.
Monitoring MRD at various points throughout treatment and remission provides important insight into a patient’s disease status in lymphoid malignancies like chronic lymphocytic leukemia, multiple myeloma, and acute lymphoblastic leukemia. Although multiple studies published in the literature have determined that achieving a negative MRD state is associated with better outcomes, there is still considerable debate among experts about the utility of an MRD-negative state in therapeutic decision-making.
Techniques to detect MRD
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
MRD testing is done using three primary methods. These methods require samples of bone marrow cells or blood cells, and one must have a bone aspiration or blood draw before one can have an MRD test. Some experts think next-generation sequencing may be a better approach for measuring MRD than flow cytometry and are the way of the future. Currently, MRD testing is being used predominantly in ALL, and its use in AML is limited for many potential reasons.
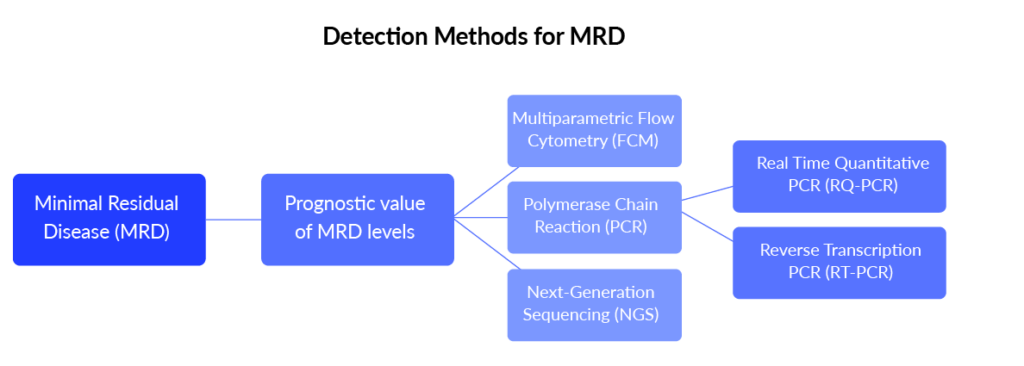
MRD detection techniques and methods include:
- Flow Cytometry: Flow cytometry uses a sample of bone marrow cells. The method uses antibodies to check for the absence or presence of important protein markers on cell surfaces. It can find cancer cells even if only one in a group of 100,000 healthy cells exists.
- Polymerase Chain Reaction (PCR): PCR looks for atypical genetic characteristics in specific segments of DNA. The test expands the DNA to count and detect atypical characteristics easier. It can be done with bone marrow or blood cells, and PCR tests can find cancer cells if there is only one in groups of 100,000 to 1 million healthy cells.
- Next-generation Sequencing (NGS): NGS testing can quickly examine stretches of DNA or RNA to look for atypical genetic characteristics. It uses bone marrow samples and can find one cancer cell in a group of 1 million healthy cells.
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
Importance of MRD in clinical decision-making
The treatment landscape for blood cancers continues to evolve, bringing new innovative medicines, such as immunotherapy, adoptive cell therapy, and others, to patients. With these advances, it is just as important that clinicians have new approaches to evaluate how well those cancer treatments work. MRD testing, used in clinical trials to assess efficacy in potential new medicines, is also being used to guide the day-to-day management of patient treatment for blood cancers. MRD tests provide an opportunity to potentially detect disease before it progresses and offer timely information for physicians and patients about how cancer treatment works at different points in a patient’s treatment journey.
A doctor may tailor when to use MRD testing based on a patient’s unique situation. For example, a doctor may recommend MRD testing:
- after the final cycle of a planned combination therapy
- after a stem cell transplant
- during treatment to confirm the depth of remission
- at the 1-year point of maintenance therapy
- at regular intervals after treatment is completed
A growing body of data suggests that MRD is prognostic for improved clinical outcomes. As such, a patient’s MRD status is now being used as an endpoint in multiple myeloma clinical trials and may potentially guide treatment decisions.
MRD testing has become an established part of the management of acute lymphoblastic leukemia (ALL), but in acute myeloid leukemia (AML), the technology still warrants validation. The European LeukemiaNet (ELN) Working Party recently published its consensus document on the topic to address issues and set new standards.
Global burden of MRD
To understand the epidemiology of MRD, one has to consider the epidemiology of hematologic cancers. According to our analysts, the incidence of blood cancers (including Acute Lymphocytic Leukemia [ALL], Acute Myelogenous Leukemia [AML], Chronic Lymphocytic Leukemia [CLL], Chronic Myelogenous Leukemia [CML], Non-Hodgkin’s Lymphoma, Hodgkin’s Lymphoma, and Multiple Myeloma) shows an increasing trend and outpacing that of solid tumors, with the number of new leukemia cases in the United States doubling in the last decade.
According to a recent analysis published by DelveInsight, in 2022, the total cases of MRD testing were around 1.2 million cases in the seven major pharmaceutical markets (7MM). The 7MM includes the United States, Germany, France, Italy, Spain, the UK, and Japan. In the 7MM, the highest number of total cases of MRD testing can be observed in the US, which accounted for 49% of total MRD testing in the 7MM
Challenge and Future perspective for MRD
According to an expert, in the community setting, MRD assessment is not part of the routine; this might be because of the lack of knowledge about the concept of MRD. The NCCN (National Comprehensive Cancer Network) is adopting the recommendation to do an MRD assessment, and dialogue between the community and academia is necessary to deliver the best care and education about MRD, not to send a blood sample for MRD and debate about the blood or bone marrow. The best sample is from bone marrow and should be the first pull, not the last. There are data comparing blood with bone marrow. The flow cytometry test requires bone marrow in the first sample, whereas bone marrow is better than blood for a next-generation sequencing (NGS) test. But the blood NGS is better than bone marrow for flow.
The ease of the MRD testing method will also uplift the adoption of the same by making the availability of MRD testing in major facilities and standardized easy sample collection for the test.
Although MRD testing can provide substantial insight, challenges still limit clinical adoption. Interpreting the results of MRD testing is complex. Whether making therapy decisions based on MRD-test results improves clinical outcomes can only be tested in randomized clinical trials; such data are currently lacking. It is important to understand that when physicians act on an MRD test result, either by giving or withholding a therapy, they might often be wrong.
However, the future of MRD testing looks promising, as ultra-sensitive MRD testing methods have already proven useful in numerous clinical studies. As research efforts continue toward standardization and more widespread adoption of the available techniques, researchers will uncover new uses and expand MRD testing strategies.
Downloads
Article in PDF
Recent Articles
- Cancer Diagnostic Market: Evaluating the Major Growth Factors and the Key Developments in the Domain
- Gilead’s TRODELVY Shows PFS Benefit in 1L Metastatic TNBC; Otsuka’s Sibeprenlimab Gets FDA Priori...
- Daiichi Sankyo’s Ezharmia; Pfizer & Sangamo Hemophilia A Gene Therapy Trial; Approval for Fe...
- CAR-T Cell Therapy aka Miraculous Technology: Mapping the Market, Approved Therapies, Competitive...
- J&J’s 2-in-1 Tablet for Prostate Cancer; FDA Approves TALVEY for Heavily Pretreated Multiple ...