Innovative Solutions, Lifesaving Possibilities: Evaluating the Artificial Organs Market Dynamics
Jul 26, 2023
Table of Contents
Over the past few years, there has been a remarkable advancement in the artificial organs market. Cutting-edge research, technological innovations, and breakthroughs in the artificial organ segment have revolutionized healthcare and extended the lives of countless individuals facing organ failure or similar impairment. Today, several different types of artificial organs are available in the market that were once hard to dream of. It has enhanced the quality of life of the affected individuals to an unimaginable extent. Globally, major MedTech and HealthTech companies are actively working to develop and deliver new artificial organs to grab the market share and generate substantial revenue. Several new and innovative artificial organs are under development and are expected to hit the market in the near future.
Advancements in Prosthetics and Artificial Organs Development
Significant work on artificial organ development was done in the early modern era. Italian anatomist Giovanni Aldini tested electrical stimulation on the human body in 1811 and found that it has the ability to manipulate muscles. Thereafter, several studies and research were done on brain interfaces and control systems for artificial organs that came later and were built on Aldini’s earlier work. Similarly, major advancements were made in the prosthetics segment only during the 20th century, with World Wars I and II increasing the demand for high-tech limb replacements. Researchers looked into the feasibility of creating more intricate organs during this time. In 1950, Dr. Charles Hufnagel successfully implanted the first mechanical heart valve, marking the first artificial organ implantation. Similarly, in 1953, Dr. John Gibbon successfully utilized the first heart-lung machine to perform open-heart surgery, setting the stage for more complex artificial organ systems. After the 1960s, there has been an influx of interest from medical device companies to develop innovative and more advanced artificial organs.
Downloads
Click Here To Get the Article in PDF
Recent Articles
- The New Buzz of Transcranial Stimulation Devices in the Neurological Disorders Market
- FDA Clears Medtronic’s New Inpen™ App; Zimmer Biomet Gets FDA Approval for Oxford® Cementless Par...
- Exploring the Impact of AI in Mental Health: How it is Going to Revolutionize Diagnosis and Treat...
- How is Active Implantable Medical Devices Market Evolving?
- Medtronic Gains CE Mark for LigaSure™ on Hugo™ Robotic System; J&J Wins FDA Nod for VARIPULSE...
The concept of artificial organs has undergone a fascinating transformation, from the 18th century to modern-day. Kidney dialysis, the artificial heart, and implantable pacemakers are some of the key segments that have gained attention. Tissue engineering and regenerative medicine have recently come to light as promising possibilities and gaining significant awareness. Researchers are working on developing different tissue engineering and regenerative artificial organs that hold immense potential to improve the lives of many patients worldwide. To lower the chance of rejection, researchers are looking into techniques to grow new organs from the patient’s own cells. This ground-breaking strategy has the potential to transform transplantation and establish artificial organs as a common form of treatment. As medical science continues to push the boundaries of innovation, the future holds the promise of even more sophisticated and lifelike artificial organs, ushering in a new era of healthcare and hope.
How Are Artificial Organs Made?
Human body organs are a complex structure and every organ is made up of two or more tissues, groups of similar cells that work together to perform a specific task. Developing an artificial organ demands intense knowledge and insights about that particular organ, its anatomy, and its function. Moreover, it requires the cooperation of professionals from several disciplines, including medicine, biology, engineering, materials science, and more. Tissue engineering and regenerative medicine also play a key role. With materials that closely resemble the composition and characteristics of actual tissues, researchers are developing biocompatible scaffolds. These scaffolds provide a framework for cell adhesion and proliferation. The scaffold is then seeded with cells, frequently made from the patient’s own tissue or stem cells. The cells are then occasionally grown in specialized bioreactors to promote tissue maturation and development. Additionally, vascularization is being added by researchers to ensure that the synthetic organ can get nutrients and blood flow.
Furthermore, advances in 3D printing technology have enabled the precise fabrication of intricate structures, further enhancing the design and customization of artificial organs. To guarantee the artificial organ’s safety, effectiveness, and compatibility with the recipient’s body, thorough testing, and validation are carried out. Artificial organs are getting more sophisticated and personalized as technology advances, opening the door to a new era of regenerative medicine and better patient outcomes.
What Are Examples of Artificial Organs?
Artificial organs describe a remarkable accomplishment of human creativity and medical innovation and immensely transform the lives of the affected individuals and their families. Cutting-edge technology, biomedical engineering, and regenerative medicine have led to the development of several live saving Artificial Organs. Some remarkable examples of artificial organs that have revolutionized the field of medicine are as follows:
Artificial Heart – One of the most well-known instances of the development of artificial organs is the artificial heart. When the heart isn’t functioning properly, a mechanical pump called a total artificial heart (TAH) is used to replace it. The artificial heart is a life-saving option for patients with severe heart failure or those awaiting heart transplantation.
Artificial Kidney – By mimicking the vital activities of the kidneys, artificial kidneys seek to give an alternative to conventional dialysis. The artificial kidney is referred to as the dialyzer and is a specialized form of filter used in hemodialysis for purifying the blood of patients whose kidney(s) has lost the ability to filter blood and excrete nitrogenous wastes.
Artificial Pancreas – Managing blood glucose levels can be a never-ending challenge for people with type 1 diabetes. The Artificial Pancreas Device System is a system of devices that closely mimics the glucose-regulating function of a healthy pancreas. The innovative artificial pancreas automates insulin distribution based on real-time blood sugar readings by fusing an insulin pump and continuous glucose monitor (CGM). Recent NIDDK-funded clinical trials have demonstrated that artificial pancreas devices regulate blood glucose levels better than alternative techniques, particularly during the night, which is difficult for many patients with type 1 diabetes, and in children as young as 6 years old.
Artificial Lung – Breathing difficulties are common in patients with severe lung disorders, and conventional treatments typically don’t help much in some cases. There is a growing demand for new technology that can take over the function of the human lung. An artificial lung (AL) is a prosthetic device that can play a key role in the oxygenation of blood and the removal of carbon dioxide from the blood. For patients with acute respiratory failure, artificial lungs, such as the Extracorporeal Membrane Oxygenation (ECMO) machine, serve as a temporary support system. By removing carbon dioxide from the body and oxygenating the blood, the ECMO system supports breathing and promotes the healing of the lungs.
Artificial Liver – The liver is essential for the body’s detoxification process and for metabolizing different chemicals. Until a suitable donor organ is found or the patient’s liver regenerates, artificial liver systems are used that help the patient’s liver to recover. They are used in patients with acute liver failure (ALF) and acute-on-chronic liver failure.
Brain-Computer Interfaces (BCIs) – Brain-computer interfaces (BCIs) are one of the most innovative technologies that help in establishing a direct line of communication between the human brain and external gadgets like computers or artificial limbs using brain signals. BCIs function by identifying, analyzing, and converting brain impulses into commands or actions that a computer can understand. Electroencephalography (EEG), invasive electrodes implanted in the brain, or other non-invasive techniques are frequently used to collect these brain signals. The Brain-Computer Interfaces are gaining significant attention and are anticipated to immensely transform the Artificial Organs market dynamics in the upcoming years with more advanced and innovative solutions.
Similarly, the eye and ear, artificial limbs, ovaries, red blood cells, testes, thymus, and trachea, are some other major organs, for which the artificial organs developments are going on. Ongoing research and technological advancements are making it possible to develop various Artificial Organs. Similarly, several new more groundbreaking advancements are expected to take place in the replacement of other body organs in the future, thereby immensely improving the lives of patients around the world.
How Much Do Artificial Organs Cost?
Unquestionably, one of the biggest obstacles to artificial organ adoption and accessibility is their high cost. The cost of artificial organs varies according to the geographical location, the healthcare facility, and the organ part required to be replaced. The manufacturing, design, and research phases include significant expenditures, which makes the end product costly. Similarly, costs are further increased by the demand for personalized solutions and the need for biocompatible materials. The development of cutting-edge technology, specialized equipment, and the requirement of skilled medical professionals and their training are frequently required for implantation and aftercare, which further increases the associated costs of artificial organs.
Owing to these direct and indirect expenses, the overall cost of obtaining and using artificial organs might be higher, making them unavailable to many patients, especially those without adequate health insurance or from disadvantaged economic backgrounds. The high cost of artificial organs highlights the urgent need for more research and development to discover more affordable strategies and technologies that can make these life-saving advancements available to a larger population, ultimately transforming the lives of those who are in critical need of such medical interventions.
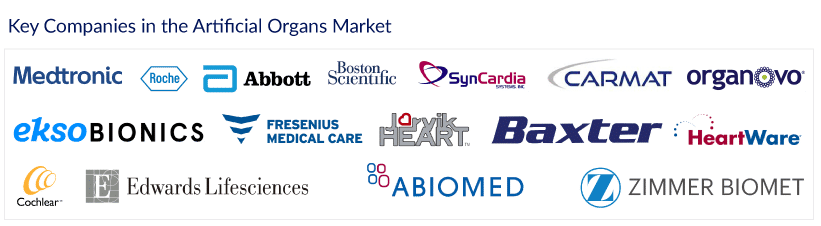
Key Companies in the Artificial Organs Market
Shortage of organs, biocompatibility and immunological rejection, and durability, are some of the key unmet needs in the artificial organs market. Globally, several major companies are actively working in the artificial organs market to overcome these challenges and grab the market share with innovative and advanced products. Medtronic, Roche, Abbott Laboratories, Boston Scientific, SynCardia Systems, Carmat, Ekso Bionics, Organovo, Fresenius Medical Care, Jarvik Heart, Baxter, HeartWare, Cochlear Limited, Edwards Lifesciences Corp, Abiomed, Berlin Heart GMBH, Ekso Bionics, Zimmer Biomet, Nipro Corporation, are key players in the artificial organs market. Owing to rising demand, growing awareness, and very high revenue prospects, several new players and startups are expected to emerge in the Artificial Organs Market.
Future Outlook of Artificial Organs Market
Artificial Organs are one of the most amazing developments in medical research. It holds the potential to transform the healthcare market outlook and prolong the lives of countless people who are suffering from organ failure or disability. Various cutting-edge research, technical advancements, and unrelenting human inventiveness are leading to more and more advancements in the Artificial Organs market with each passing day.
As per DelveInsight, the increasing prevalence of chronic diseases, organ shortage and transplant waiting lists, advancements in technology and biomedical engineering, favorable reimbursement policies, aging population, are some of the key factors expected to immensely drive the Artificial Organs Market outlook in the upcoming years. Increasing healthcare expenditure and the active participation of the major MedTech giants in new product development are also providing momentum to artificial organ market growth. However, high cost and regulatory & safety issues are the key areas that need to be addressed for a wider acceptance of these innovations and life-saving products.
Downloads
Article in PDF
Recent Articles
- Alcon’s 510(k) Clearance From the FDA; Globus Medical Received FDA Clearance; UK Pioneers F...
- The New Buzz of Transcranial Stimulation Devices in the Neurological Disorders Market
- Glucotrack Secures Ethical Approval for Extended Clinical Trial of Continuous Blood Glucose Monit...
- Top Biosurgery Applications Revolutionizing Modern Medicine
- Suneva Medical-Viveon Health merger update; Smith+Nephew acquires Engage Surgical; Abiomed’...